

It would cause Medicare beneficiaries to lose no-cost access to lifesaving vaccines.

By Jill Rosenthal
Director, Public Health
The Center for American Progress

By Marquisha Johns, J.D.
Associate Director, Public Health
The Center for American Progress
Introduction
As temperatures cool this fall, Americans can expect to see a rise in vaccine-preventable respiratory diseases that are more common in colder months. Critically, the Inflation Reduction Act (IRA) of 2022 provided a mechanism to protect Medicare beneficiaries from vaccine-preventable diseases by requiring Medicare drug plans—also known as prescription drug, or Part D, plans—to make vaccines recommended by the Advisory Committee on Immunization Practices free for enrollees. The requirement, which went into effect in January 2023, aligns with an existing Affordable Care Act (ACA) requirement for most private health plans and increases equity in vaccine coverage by expanding access to vaccines at no cost for older Americans and people with disabilities.
Vaccination is considered one of the most cost-effective health care and public health interventions, and there is strong evidence that reducing out-of-pocket costs improves vaccination rates. The IRA requirement, for one, guarantees nearly 54 million Medicare Part D beneficiaries access to free vaccines.
However, Project 2025—the Heritage Foundation’s radical policy agenda that seeks to give far-right politicians, judges, and corporations more control over Americans’ lives—calls for the Inflation Reduction Act’s repeal. Along with the many IRA benefits that would disappear if the law were repealed, Medicare Part D beneficiaries would lose their access to no-cost vaccines, a vital benefit that enables them to stay healthy and avoid contracting diseases. Repealing the IRA would also exacerbate racial, ethnic and economic inequities.
Free Vaccines Are Important for Helping Medicare Enrollees Stay Healthy
Vaccination effectively prevents infectious disease, disability, and death—and, in some cases, eliminates diseases altogether. In fact, vaccines are the best protection against preventable diseases.
Vaccines are especially critical for older Americans—who are mostly covered by the Medicare program—because they have weakened immune systems, which increases susceptibility to infectious disease. In 2023, 88 percent of the 51.9 million Medicare beneficiaries who were enrolled in Medicare Part D at that time were ages 65 and older. The Centers for Disease Control and Prevention (CDC) recommends that older adults receive a variety of vaccines, including vaccines to prevent pneumococcal disease, shingles, RSV, COVID-19 and seasonal flu. In addition, vaccine boosters to prevent tetanus and diphtheria (Td) or tetanus, diphtheria, and pertussis (Tdap) are recommended every 10 years.
The CDC recommends that people ages 50 and older get vaccinated to prevent shingles, which can cause debilitating pain, itching, or tingling and potentially long-term nerve pain. A two-shot dose of the shingles vaccine is more than 90 percent effective at preventing shingles among adults ages 50 and older who have healthy immune systems. Moreover, new research from the University of Oxford found that the shingles vaccine reduces the risk of dementia by at least 17 percent. Before the shingles vaccine was made free under the IRA, it cost Medicare Part D enrollees $77 on average.
Respiratory syncytial virus (RSV) can cause an infection of the lungs and respiratory tract. It can cause serious illness in older adults, and very severe cases may require support with eating and breathing. Each year, there are nearly 160,000 hospitalizations and 10,000 deaths related to RSV among older adults, with medical costs of up to $3.4 billion. The U.S. Food and Drug Administration approved new vaccines for RSV in 2023, and they are now recommended for all adults ages 75 and older—and for those ages 60 to 74 at risk of severe RSV disease. These vaccines are up to 83 percent effective in preventing RSV hospitalizations and emergency department visits. In 2023, the RSV vaccine’s first year on the market, 12.6 percent of Medicare Part D enrollees received it for free due to the IRA’s no-cost provision.
Project 2025’s Plan Would Put Older Adults at Risk
Data show that many Medicare enrollees are benefiting from the IRA’s no-cost vaccine requirement: According to the U.S. Department of Health and Human Services’ Office of the Assistant Secretary for Planning and Evaluation (ASPE), in 2023, 10.3 million people, or 20 percent of all Medicare enrollees, received a recommended free vaccine under Medicare Part D—up from only 3.4 million, or 7 percent of enrollees, in 2021. During this period, the shingles vaccine rate increased by 42 percent, the Tdap vaccine rate increased by 114 percent, and 6.5 million enrollees received the new RSV vaccine.
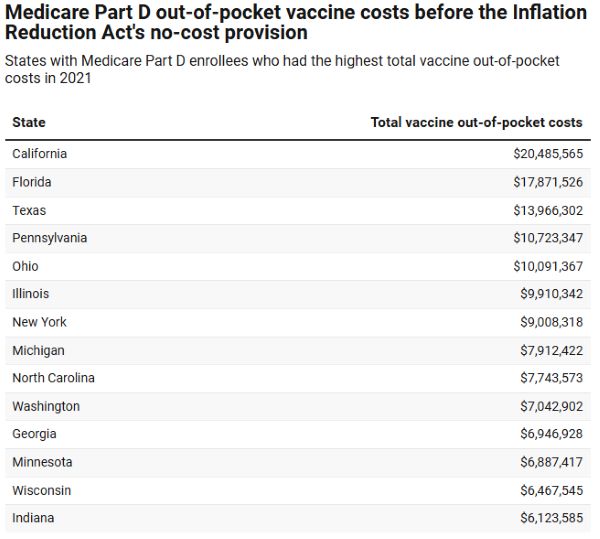
Thanks to the IRA’s no-cost vaccine provision, Medicare beneficiaries saved more than $400 million in out-of-pocket vaccine costs—excluding RSV—in 2023. Before the IRA eliminated vaccine cost-sharing, Medicare Part D enrollees spent $234 million, or $70 per person, in out-of-pocket vaccine costs in 2021. Beneficiaries in just 15 states accounted for nearly 63 percent of this out-of-pocket spending. (see Table 1) Cost-sharing at the time varied widely across covered vaccines, with average out-of-pocket costs between approximately $20 for the tetanus/diphtheria vaccine and $77 for the shingles vaccine. Some enrollees even paid as much as $195 for a single vaccine in 2021.
Black, Latino, and Lower-Income Adults Are Most Harmed
Research has long established that cost-sharing is a deterrent to vaccination. This holds true among the Medicare population, where the median income is $36,000 per person and most beneficiaries have limited financial resources for health care expenses. In fact, one study found that fewer Medicare enrollees received the shingles vaccine when the average out-of-pocket costs for the vaccine increased. Conversely, uptake of the shingles vaccine among enrollees increased by up to 60 percent when the vaccine was free.
Older Black and Latino adults would be most harmed by Project 2025’s plan to repeal the IRA’s Medicare Part D no-cost vaccine requirement. According to IQVIA research, Black (42 percent) and Hispanic (44 percent) patients are more likely than white patients (28 percent) to forgo payer-approved vaccines when asked to pay a copay of between $10 and $40, a common copay range for Medicare Part D drugs. In 2021, Black and Hispanic adults ages 65 and older were less likely to have received a pneumococcal vaccine and those ages 60 and older were less likely to have received a shingles vaccine, compared with their white peers.
Due to structural racism, Black and Latino older adults face a variety of barriers to vaccination, in addition to out-of-pocket costs, that affect their uptake of vaccines. Such barriers include more limited access to health care providers and pharmacies, language barriers, and reported discrimination in health care settings.
Conclusion
Among Project 2025’s far-reaching effects, its plan to repeal the Inflation Reduction Act and eliminate no-cost vaccine coverage for Medicare beneficiaries would increase costs for Medicare enrollees and reverse gains in vaccine uptake. These losses would be felt most acutely by older Black and Latino adults as well as older adults with lower incomes and those in states with the highest out-of-pocket vaccine costs prior to the IRA. Reimposing barriers to accessing vaccines would threaten the health and economic security of these vulnerable Americans.
Originally published by The Center for American Progress, 09.11.2024, republished with permission educational, for non-commercial purposes.


