Getty Images
Parents of young children support measles, mumps and rubella vaccine requirements. There are not major partisan divisions on these issues.
By (left-to-right) Dr. Cary Funk, Dr. Brian Kennedy, and Meg Hefferon / 02.02.2017
Funk: Director, Science and Society Research
Kennedy: Research Associate
Hefferon: Research Assistant
Pew Research Center
Introduction
Most Americans support requiring the measles, mumps and rubella vaccine for public school children in order to protect public health. They see high preventive health benefits of such vaccines, and low risk of side effects, and they consider the benefits of the vaccine to outweigh the risks.
Yet, public concerns about childhood vaccines linger in the public discourse, often linked to a now discredited and retracted research study published nearly two decades ago that raised questions about a possible link between the measles, mumps and rubella vaccine and autism. Despite assurances of vaccine safety from the Centers for Disease Control and Prevention, the American Academy of Pediatrics and a host of other scientific bodies that the measles, mumps and rubella (MMR) vaccine does not cause autism, a number of prominent figures have expressed concerns about the safety of childhood vaccines. President Donald Trump raised questions about the safety of childhood vaccines on the campaign trail and during the transition period met with Robert Kennedy Jr. reportedly about the possibility of leading a commission on vaccine safety and scientific integrity. Kennedy edited a book that argues that a preservative used in some vaccines causes neurological disorders, including autism.1
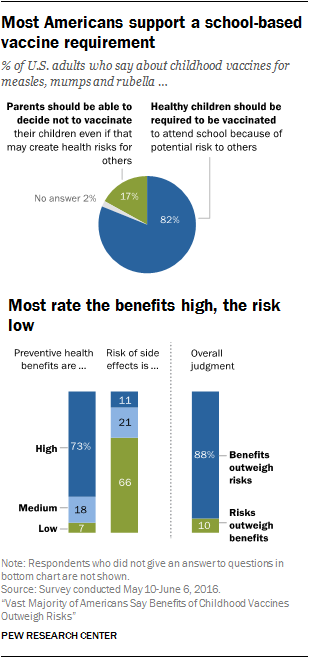
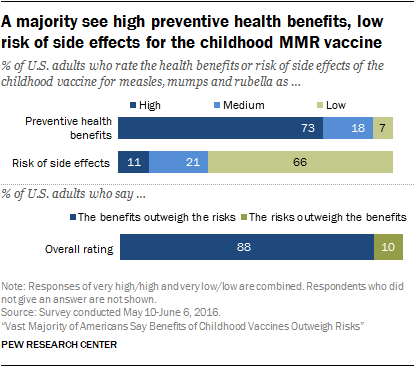
A new Pew Research Center survey conducted prior to the election finds the “vaccine hesitant” views expressed by Trump and other public figures to be at odds with most Americans’ views. An overwhelming majority of Americans (82%) support requiring all healthy schoolchildren to be vaccinated for measles, mumps and rubella. Some 73% of Americans see high preventive health benefits from use of the MMR vaccine, and 66% believe there is a low risk of side effects from the vaccine. Overall, 88% believe that the benefits of these inoculations outweigh the risks.
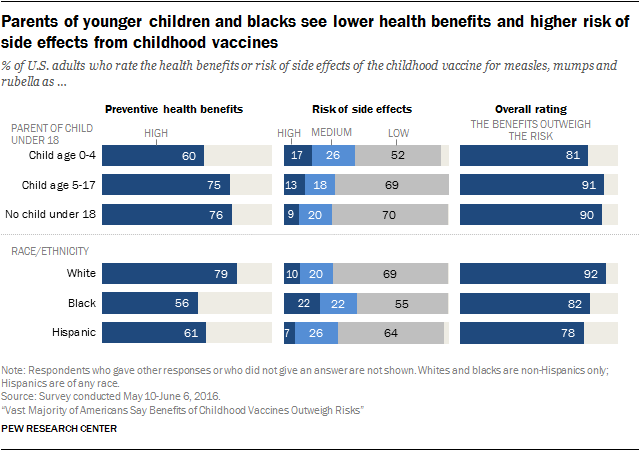
But there are several groups with comparatively more concern about the safety of the measles, mumps and rubella vaccine. Foremost among them are parents of children ages 0 to 4 who have recently faced or will soon face a decision about whether to follow the recommended immunization schedule for measles, mumps and rubella starting when their children are between 12 and 15 months old. Six-in-ten (60%) parents with children ages 0 to 4 see the preventive health benefits of the MMR vaccine as high, compared with 75% of parents with school-age children (ages 5-17) and 76% of people with no children under age 18. About half (52%) of parents with children ages 0 to 4 say the risk of side effects from the MMR vaccine is low, 43% of this group says the risk is medium or high. By comparison, 70% of those with no minor age children say the risk of side effects is low, and 29% say the risk is medium or worse.
In addition, blacks consider the risk of side effects from the MMR vaccine to be higher and the benefits lower than other Americans. There are also generational differences with adults under age 30 less convinced that the MMR vaccine brings high preventive health benefits. People’s use of alternative and conventional medicine is linked with their beliefs about the MMR vaccine; those who report never taking over-the-counter cold or flu medication and those who have used alternative medicine instead of conventional medicine see higher risk from the MMR vaccine.
People with low knowledge about science are also less likely to see high preventive health benefits from vaccines (55% compared with 91% of those high in science knowledge).2 In addition, they are more likely to consider the risk of side effects to be at least “medium” or worse (47% vs. 19% of those with high science knowledge.) Similarly, the 68% majority of Americans who do not correctly recognize the definition for “herd immunity” are less likely to rate the benefits of the MMR vaccine as high and comparatively more likely to see the risk of side effects as at least medium. (Herd immunity refers to the health benefits that occur when most people in a population have been vaccinated.) This group is equally likely as those who correctly recognize the term “herd immunity” to support a requirement for all children in public schools to be vaccinated.
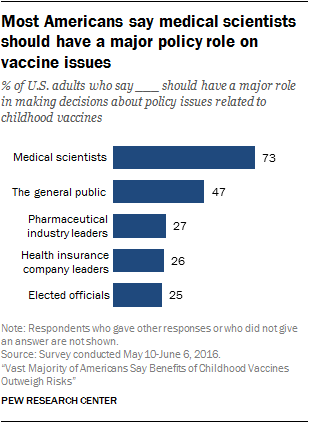
Nonetheless, public views of medical scientists and their research related to childhood vaccines are broadly positive regardless of parent status, race, ethnicity and experience using alternative medicine. Fully 73% of U.S. adults believe that medical scientists should have a major role in policy decisions related to childhood vaccines. In addition, a 55% majority say they trust information from medical scientists a lot to give a full and accurate picture of the health effects of vaccines. At the same time people are less trusting of other groups about this issue. For example, just 13% trust information from pharmaceutical industry leaders about the health effects of the MMR vaccine a lot. People with high science knowledge are especially positive in their views of medical scientists and research on childhood vaccines. Younger adults, ages 18 to 29, are a bit more skeptical than older age groups about medical scientists and their work on childhood vaccines.
The new Pew Research Center survey finds Republicans (including independents who lean Republican) hold roughly the same views as Democrats (including leaning Democrats) about the benefits and risks of the MMR vaccine, consistent with a 2015 Pew Research Center survey on this topic. Republicans and Democrats (including those who lean to either party) are about equally likely to support a school-based vaccine requirement. However, political conservatives are slightly more likely than either moderates or liberals to say that parents should be able to decide not to have their children vaccinated, though majorities of all ideology groups support requiring the measles, mumps and rubella vaccine for all children in public schools because of the potential health risk to others.
These are some of the findings from a Pew Research Center survey conducted among a nationally representative sample of 1,549 adults, ages 18 or older from May 10-June 6, 2016. This is the third in a series of reports on public views about science-related issues and public trust in scientists working on these issues. The margin of sampling error based on the full sample is plus or minus 4.0 percentage points. For details, see the Methodology.
82% of Americans say the measles, mumps and rubella vaccine should be required for healthy schoolchildren in order to reduce public health risk.
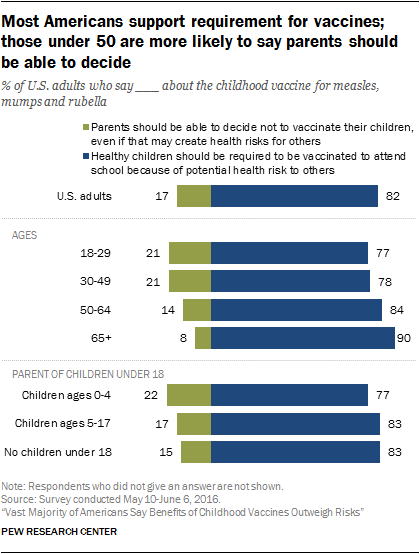
An overwhelming majority of Americans (82%) support having a school-based requirement that healthy children be vaccinated for measles, mumps and rubella. Older adults, ages 65 and older, are especially strong in their support for requiring the MMR vaccine.
Seniors, ages 65 and older, support a school-based requirement for the MMR vaccine by a margin of 90% to 8% who say that parents should be able to decide this. Smaller majorities of younger age groups support a school requirement for the MMR vaccine.
Parents of young children, parents of school-age children and those with no minor age children hold roughly similar views on this issue, with a majority of all three groups saying that healthy schoolchildren should be required to be vaccinated because of the health risk to others when children are not vaccinated. Some 77% of parents with children ages 0 to 4 say that healthy children should be required to be vaccinated for the MMR because of the potential health risk to others when children are not vaccinated, while 22% of this group says parents should be able to decide not to have their children vaccinated even if that creates health risks for others.
Conservatives (25%) are a bit more likely than either moderates (15%) or liberals (9%) to say that parents should be able to decide not to have their children vaccinated even if that creates health risks for others. At least seven-in-ten of all three ideology groups say that the MMR vaccine should be required for healthy schoolchildren, however. There are no significant differences in views about this issue by political party in this survey.
White evangelical Protestants and the religiously unaffiliated tend to express a bit less support for requiring the MMR vaccine and comparatively more support for allowing parents to decide not to have their children vaccinated. Majorities of all major religious groups, though, say that the MMR vaccine should be required for healthy school children.
Health practices related to conventional and alternative medicine linked to people’s views about childhood vaccines.
Two additional groups have notably different views about childhood vaccines than others. One is the 20% of adults who report they have used alternative medicine instead of traditional medicine. The other is 8% of Americans who report that they never take over-the-counter medications.
Alternative medicine is a broad category including herbal dietary supplements, acupuncture, chiropractic, energy therapies and other therapies that are not part of standard conventional (here also called traditional) Western-based medical care. Many of these alternative therapies have uncertain healing effects although some techniques have been shown to help relieve pain and nausea and are used as complementary treatments in addition to conventional, standard medical care.
The new Pew Research Center survey finds half of U.S. adults (50%) report never having used alternative medicine; one-fifth (20%) say they have used alternative medicine instead of conventional treatment, and 29% have used it in addition to conventional treatment.3
Another indicator of people’s use of conventional medicine involves their use of over-the-counter cold and flu medications. Some 41% of Americans report that they take such medications as soon they experience cold or flu symptoms, 49% say they wait to take such medications until their cold or flu symptoms worsen, and 8% report that they never take over-the-counter medications for cold or flu symptoms.
The minority of Americans who report never using over-the-counter medications for cold or flu symptoms and those who have used alternative medicine instead of conventional treatment are comparatively more likely to think that parents should be able to decide whether to have their children vaccinated even if that decision means increased health risk for others. Most in these groups, however, say that healthy children should be required to be vaccinated in order to attend public schools.
Overall, public perceptions of the benefits and risks of the measles, mumps and rubella vaccine are strongly positive. Some 73% of U.S. adults rate the preventive health benefits of the MMR vaccine as high, and 66% of the public says the risk of side effects from the vaccine is low. About a third (32%) say the risks are medium or high. When considering the trade-offs, fully 88% of Americans say the benefits of the MMR vaccine outweigh any risks, while just one-in-ten say the risks outweigh the benefits.
Parents with children through age 4 are comparatively less convinced that the MMR vaccine has high preventive health benefits and are more concerned about the risk of side effects. Six-in-ten (60%) of those with a child ages 0 to 4 say the benefits are high, compared with 76% of those with no children under age 18. Some 43% of parents with young children (ages 0 to 4) say the risk of side effects from the MMR vaccine is at least medium, compared with 29% of those with no minor-age children.
Blacks (56%) and Hispanics (61%) are less inclined than are whites (79%) to see the preventive health benefits of the MMR vaccine as high. Blacks also tend to see the risk of side effects from the MMR vaccine as at least medium compared with whites (44% of blacks vs. 30% of whites say this).4
People with high science knowledge, higher levels of education and higher family income are especially likely to rate the preventive health benefits of the MMR vaccine as high and the risk of side effects as low. For example, 91% of those with high science knowledge say the health benefits of the MMR vaccine are high, compared with 55% of those with low science knowledge. Just 19% of those with high science knowledge consider the risk of side effects from the MMR vaccine to be at least medium, compared with 47% of those with low science knowledge.
Reports that affluent communities have lower vaccination rates lead some to speculate that people with higher incomes hold more concerns about the safety of the MMR vaccine. The Pew Research Center survey finds, however, that people with higher family incomes tend to rate the risk of side effects from the MMR vaccine as low. Those with higher family incomes are especially strong in their support for a requirement that all children be required to be vaccinated against MMR in order to attend public schools.
The 8% of Americans who report never using over-the-counter medications for cold or flu symptoms are comparatively less convinced of the preventive health benefits (59% say the benefits are high, compared with 75% among all who take such medications) and more concerned about the risk of side effects from the MMR vaccine (49% say the risk of side effects are at least medium, compared with 31% of all who take such medications). There is a similar, though less pronounced, pattern among those who have used alternative medicine in lieu of conventional medicine compared with other Americans.
There are not noteworthy differences in people’s perceptions of the benefits and risks associated with the MMR vaccine by gender, religious affiliation or political groups.
Trust in medical scientists and their research
Public perceptions of medical scientists and their research are broadly positive. Some 55% of Americans perceive strong consensus among medical scientists that the measles, mumps and rubella vaccine is safe for healthy children. Nearly half of Americans (47%) say that medical scientists understand very well the risks and benefits of the MMR vaccine, 43% say medical scientists understand this fairly well and just one-in-ten (10%) say medical scientists do not understand this at all or not too well.
A 55% majority of Americans trust information from medical scientists a lot to give a full and accurate picture of the health effects of vaccines. Public trust in information from other groups is much lower including: pharmaceutical industry leaders (13%), people from holistic or alternative health groups (9%), the news media (8%) and elected officials (6%).
Some 52% say that scientists’ research on childhood vaccines is influenced by the best available evidence most of the time, and 55% say such research is influenced by scientists’ concern for the best interests of children’s health most of the time. Smaller shares say that researchers’ desire to help their industries or to advance their own careers influences research on childhood vaccines most of the time.
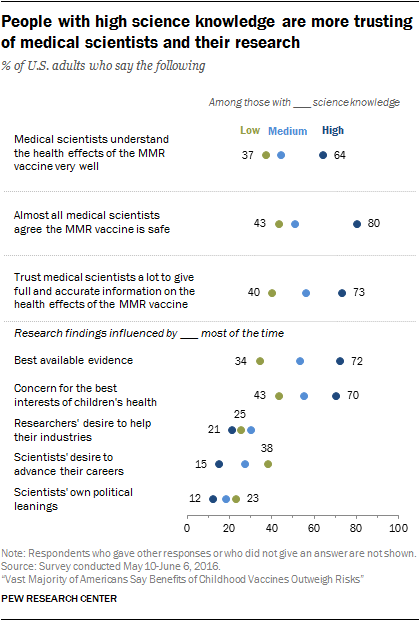
Americans’ views about medical scientists and their work, however, vary widely by people’s level of knowledge about science. People with high science knowledge, based on a nine-item index, tend to be positive and trusting of medical scientists and their work on childhood vaccines. By contrast, a minority of those low in science knowledge perceive medical scientists as understanding the risks and benefits of the MMR vaccine very well, trust information from medical scientists a lot, or think that the best available evidence influences medical research on childhood vaccines most of the time.
In addition, there are modest generational differences in views about medical scientists. Younger adults, ages 18 to 29, are less inclined than older adults to see medical scientists and their research in a positive light.
Most Americans support a policy role for medical scientists on vaccine issues.
While there is considerable variation in Americans’ views about medical scientists’ understanding of childhood vaccines, most Americans think medical scientists should have a role in policy decisions related to childhood vaccines. Fully 73% of U.S. adults think that medical scientists should have a major role, 19% think they should have a minor role in such policy-making decisions, and 7% think medical scientists should have no role in vaccine policymaking.
Far fewer Americans say that other groups should have a major role in policy decisions on these issues, including the general public (47%), pharmaceutical industry leaders (27%), health insurance company leaders (26%) or elected officials (25%).
Most Americans express confidence in medical scientists to act in the public interest
Asked about a wide range of leaders and institutions, the military, medical scientists, and scientists, in general, received the most votes of confidence when it comes to acting in the best interests of the public. On the flip side, majorities of the public have little confidence in the news media, business leaders and elected officials. Public confidence in K-12 school leaders and religious leaders to act in the public’s best interest falls in the middle, as shown in a 2016 report from the same Pew Research Center survey.
Fully 84% of Americans say they have a great deal (24%) or a fair amount (60%) of confidence in medical scientists to act in the public’s best interests. About eight-in-ten or more report at least a fair amount of confidence in medical scientists to act in the public interest across a range of subgroups including gender, age, parents, race and ethnicity, education, political party and ideology and religion.
Other key findings in the report include:
- Nearly half of Americans (48%) say the health of children in the U.S. as a whole has declined over the past two decades, a smaller share (31%) say it has gotten better and a fifth (20%) say children’s health has stayed about the same. People’s perceptions of adult health over the past 20 years are slightly more negative than positive as well. People ages 65 and older are the only age group in which a plurality sees the public health of both children and adults as better today than it was two decades ago.
- Most Americans see reports of conflicting health studies as part of the march of research progress. Fully 74% of adults say conflicting news reports about disease prevention are understandable because “new research is constantly improving our understanding,” while 23% of adults say such research “cannot really be trusted because so many studies conflict with each other.”
- A 61% majority of Americans give the media positive marks, overall, for their coverage of issues related to the measles, mumps and rubella vaccine. Half of Americans say they follow news about childhood vaccines very (13%) or somewhat (37%) closely. Fully 73% of this media attentive group says the media do a good job covering issues about childhood vaccines, and 27% says the media do a bad job on this. Parents of children ages 0 to 4 do not differ from other adults in their judgments about media coverage of the MMR vaccine.
- Most people who have seen a health care provider for treatment needs in the past year say the provider listened to their concerns and cared about their well-being. Roughly six-in-ten Americans (63%) report that they have gone to a health care provider for an illness or medical condition in the past year, and 36% have not. Fully 87% of those who have been to a health care provider within the past year felt their description of their symptoms or concerns were carefully listened to, 84% felt the health care provider “really cared about [their] health and well-being” and 80% say they got all the information they needed for further treatment and at-home care. Only 23% of this group reports feeling rushed by the health care provider, and only 15% felt confused about the instructions they received for further treatment or at-home care.
- When it comes to making decisions about treatment for a serious health problem, three-in-ten adults (30%) say they “just ask a doctor for advice,“ while some 68% of Americans say they also do their own research, either to check for other treatment options (21% of U.S. adults), to understand potential side effects for a recommended treatment (9% of U.S. adults) or simply to learn more about the recommended treatment (36% of U.S. adults).
Americans’ Views about Public Health and Health Studies in the News
Overall, asked whether public health is better, worse or stable over the past few decades, Americans tilt toward viewing health outcomes in the U.S. as declining compared with 20 years ago. A plurality of U.S. adults say that children’s and adults’ health are both worse today than they were two decades ago. This view is shared among all age groups except seniors; about half of those ages 65 and older think that the health of both children and adults is better today than it was 20 years ago.
While the general public tends to see a mix of factors as important for health, more Americans say healthy eating and exercise are very important for preventing serious disease than say genetic factors or safe and healthy housing conditions are important determinants of health. The public’s beliefs about the factors in disease prevention are similar across age, gender and income groups.
Many Americans pay attention to health information in the media about ways people can protect themselves from the risk of serious disease. Observers have sometimes worried that back-and-forth contradictory media reports about health confuse people, or worse, foster distrust in health and medical studies. The Pew Research Center survey finds that while most Americans report seeing news reports whose advice about disease prevention conflicts with earlier reports, they see the back and forth as a sign of continued research progress. A majority of Americans say it makes sense that news reports over time contain conflicting advice because new research is constantly improving our understanding of disease. A minority of Americans say that such research cannot be trusted because so many studies conflict.
More Americans today view public health as declining than improving
The American public is more pessimistic than optimistic in its assessments of public health today. Nearly half (48%) of Americans believe children’s health, as a whole, is worse today than it was 20 years ago; by comparison, a smaller share, 31%, believe children’s health is better today. One-in-five adults (20%) say children’s health is about the same as it was.
People’s views of change in adult health over the past two decades are similarly more negative than positive. Some 42% of Americans say the health of the adult population in the country is generally worse today, 33% say it is better and 24% say it is about the same as it was 20 years ago.
There are large differences by age in people’s views about public health, suggesting that generational experiences influence these perceptions. Seniors are the only age group in which more people see public health as better rather than the same or worse today. About half (49%) of adults ages 65 and older say that children’s health is generally better today than it was 20 years ago. In comparison, 27% of adults ages 18 to 49 say that children’s health is better today than it was 20 years ago.
And, fully half (53%) of people ages 65 and older say that adult health is better today than it was 20 years ago. In contrast, Americans in younger age groups are more likely to say the health of adults is worse today.
The public sees healthy eating and exercise as key factors in preventing serious disease
Americans are most likely to highlight controllable factors, especially diet and exercise, as important for preventing serious disease. Seven-in-ten adults say that healthy eating habits are very important in preventing a person from getting serious diseases such as cancer or heart disease. Two-thirds (66%) of Americans say getting enough physical exercise is very important in disease prevention.
Smaller shares, though still a majority, say genetics and hereditary factors (55%) or safe and healthy housing conditions (55%) are very important factors to prevent serious diseases, such as cancer and heart disease.
Beliefs about the factors in disease prevention are similar across gender, age and income. But, women are somewhat more likely than men to say that safe housing conditions (61% vs. 48%) as well as genetics and hereditary factors (59% vs. 50%) are very important for preventing serious diseases. And those with low family incomes are more likely to say that safe and healthy housing conditions are very important for preventing serious diseases (61% of those with incomes of less than $30,000 annually compared with 48% of those with family incomes of $100,000 or higher).
Conflicting news reports on disease prevention abound, but most Americans see such stories as part of the research process
Most Americans pay attention to stories about how to prevent serious diseases such as cancer or heart disease. Most members of the public (55%) say they hear or read news stories about the ways people can protect themselves from the risk of serious diseases every day (16%) or a few times a week (40%). An additional 28% report they see such news stories a few times a month; 15% say they see such news stories less often than that.
Older Americans are especially likely to follow health news about disease prevention. About two-thirds (65%) of adults ages 50 and older say they hear or read media reports on disease prevention at least a few times a week. By comparison, some 47% of those ages 18 to 49 say they follow news on this topic at least a few times a week.5
People who follow health news regularly are especially likely to say they hear or read news stories about disease prevention that conflict with prior stories. About half (49%) of those who see media reports about disease prevention every day also say they see conflicting news stories about this “all the time.” In comparison, just 13% of all U.S. adults say they hear or read media stories about disease prevention that conflict with prior stories “all the time.”
Some in the science community have worried that news reports of research with conflicting findings about disease prevention might undermine public trust in science.6 While most people are aware of conflicting health studies in the media, most see it as a sign of research progress. Some 74% of U.S. adults say it makes sense that findings conflict because “new research is constantly improving our understanding about ways to protect people from the risk of serious disease.” A smaller share (23%), however, says that “research about ways people can protect themselves from the risk of serious disease cannot really be trusted because so many studies conflict with each other.”
People’s views about contradictory health studies tend to vary depending on their level of science knowledge. An overwhelming majority of those with high science knowledge say studies with findings that conflict with prior research are a sign that understanding of disease prevention is improving (85%). A smaller majority of those with low science knowledge say the same (65%), while 31% say that the research cannot really be trusted because so many studies conflict with each other.
Pew Research Center’s 2016 companion report on public views about food science found a similar pattern. A majority of Americans said they see conflicting media stories about the health effects of food. Some 61% of Americans said that, “new research is constantly improving our understanding about the health effects of what people eat and drink, so it makes sense that these findings conflict with prior studies,” while fewer (37%) said, “research about the health effects of what people eat and drink cannot really be trusted because so many studies conflict with each other.” Similarly, people with lower levels of science knowledge were particularly likely to say that such studies could not be trusted because so many studies conflict.
Americans’ Health Care Behaviors and Use of Conventional and Alternative Medicine
Americans who have seen a health care provider in the past year for treatment of an illness or medical condition hold largely positive views of their experience. Most of those receiving care felt that their description of their symptoms was carefully listened to, that their health care provider really cared about their health and well-being and that they received the information they needed for their treatment or home-based care. Only a minority of this group reports having felt rushed by their health care provider or confused about the instructions they received for at-home care or treatment needs.
At the same time, a majority of Americans say that when they make decisions about treatment for a serious health problem, they do their own research in addition to seeking advice from a doctor or other health care provider. Some of those who report doing their own research say they are aiming simply to learn more about the provider’s recommendations, while other people say they do so to check for other treatment options or to learn about potential side effects of the recommended treatment.
About half of Americans report having tried some form of alternative medicine, such as herbal remedies, acupuncture, chiropractic treatment or energy therapies, at some point during their lifetime. About a fifth of Americans say they have tried alternative medicine instead of conventional medicine; and, roughly three-in-ten adults have tried alternative medicine in conjunction with conventional medical treatment. In addition, about one-in-twelve Americans report that they never use over-the-counter medications when experiencing cold or flu symptoms, while the remainder say they either take such medications right away or wait until their symptoms worsen. People who have used alternative medicine instead of conventional medicine and those who never take over-the counter medications are less likely to have a primary care provider, to have had a flu shot and to have had a preventive care checkup in the past year.
Health care options can vary widely from community to community. A minority of the public says that access to quality health care is a big problem in their local area. People’s views about access to quality health care are linked with community size and type as well as family income.
Most Americans berate themselves for not getting enough exercise. Nearly eight-in-ten Americans say they “should probably be getting more exercise.” A majority of those who say they exercise “a few times a week” believe they should be getting more exercise than they do. By contrast, most of those who exercise daily say they get about as much exercise as they should. Regardless, fewer than one-in-six adults describe their lifestyle as “very healthy”; most see themselves as having a “somewhat” healthy lifestyle.
Roughly half of Americans report that they exercise at least a few times each week, but three-quarters of Americans believe they should be getting more exercise
About half of Americans say they exercise every day (15%) or a few times a week (38%). Some 47% of U.S. adults say they exercise no more than a few times a month.
At the same time, 79% of Americans believe that they should probably be getting more physical exercise; only 20% say they get as much exercise as they should.
While most people who report exercising every day judge themselves to be getting as much exercise as they should (65%), some 35% of this group thinks they, too, should be getting more exercise.
Previous surveys conducted by telephone, including one by Pew Research Center in 2006, also found a majority of Americans said they should be getting more exercise. One factor in these perceptions of self-failings may be the sense that exercise is important for lessening the risk of disease. Two-thirds (66%) of Americans in this new Pew Research Center survey say getting enough exercise is very important for preventing the risk of serious disease, and an additional 29% say it is somewhat important.
Most Americans see themselves as having a “somewhat healthy lifestyle”
Most Americans judge themselves to be living a somewhat (66%) or very (14%) healthy lifestyle. About two-in-ten Americans (19%) describe their lifestyle as not very or not at all healthy.
Non-smokers and those who exercise regularly are more likely to see themselves as following a very or somewhat healthy lifestyle, as do adults ages 50 and older.
Some 36% of Americans who exercise daily say that they live a very healthy lifestyle, compared with just 6% of those who exercise a few times a month or less often.
Similarly, 18% of people who have never been cigarette smokers describe themselves as having a very healthy lifestyle, compared with 6% of current smokers.
One-quarter (25%) of adults ages 65 and older consider themselves to have a very healthy lifestyle; just 9% of 18- to 29-year-olds say the same.
Men and women are about equally likely to see themselves as following a healthy lifestyle.
People following healthy lifestyles tend to have social networks contacts who do the same
One-in-five Americans say that most of their closest family and friends live a healthy lifestyle. An additional 56% say some of them do, while 20% say only a few do and just 4% say none of their friends or relatives live a healthy lifestyle.
Fully 46% of people who see themselves as following a very healthy lifestyle say that most of their close family and friends do the same. In contrast, just 5% of people who describe their own lifestyle as not very or not at all healthy say that most of their close family and friends follow a very healthy lifestyle.
Public views about access to quality health care vary across community types
Health care options can vary widely from community to community. People’s views about access to quality health care are linked with community size and type as well as family income. Overall, some 27% of Americans say that access to quality health care is a big problem in their community, 42% call it a small problem and three-in-ten (30%) say this is not a problem in their area.
Americans living in rural (33%) and urban (30%) communities are more inclined than those living in suburban communities (23%) to say access to quality health care is a big problem where they live.
Just 14% of those with a family income of $100,000 or more say access to quality health care is a big problem, while a much larger share (43%) say this is not a problem in their local community. In contrast, 35% of people with a household income of less than $30,000 say access to quality health care is a big problem in their community. Just one-quarter (25%) of those with lower incomes say access to quality health care is not a problem.
Women are slightly more likely than men to see access to quality health care as a big problem where they live (33% compared with 21% among men).
By comparison, more Americans consider the availability of jobs to be a big problem in their local community (44%) than say the same about access to quality health care (27%). A similar share of Americans (26%) say the quality of K-12 education in public schools is a big problem where they live.
Most people report positive experiences when receiving health care treatment
Roughly six-in-ten Americans (63%) report that they have gone to a health care provider for an illness or medical condition in the past year, while 36% have not.
The vast majority of people who have seen a health care provider for an illness or medical condition in the past year report positive experiences. Fully 87% of those who have been to a health care provider within the past year felt their concerns or descriptions of symptoms were carefully listened to, 84% say they felt their health care provider “really cared about (their) health and well-being” and 80% say they got all the information they needed for further treatment and at-home care. Only 23% of this group report feeling rushed by the health care provider and only 15% felt confused about the instructions they received for further treatment or at-home care.
Some 23% of those with a high school diploma or less schooling who saw a health care provider in the past year say they felt confused about follow-up instructions for care; that figure is only slightly higher than the 15% of those with a postgraduate degree who say the same. People across demographic groups, including gender, age, race and ethnicity, as well as those with a regular health care provider and those without, give broadly positive assessments of their health care treatment visits.
People’s use of conventional and alternative medicine tie with their use of preventive health care
The Pew Research Center survey included a few questions about people’s habits and practices in using conventional and alternative medicine; these behaviors correlate with their use of preventive care and, as shown in the next chapter, their views about the risks and benefits of childhood vaccines. One measure comes from people’s use of alternative medicine, particularly if used instead of “traditional,” Western-based conventional medicine. Another measure comes from people’s practices regarding their use of over-the-counter medications for cold or flu symptoms.
A fifth of Americans say they have tried alternative treatments in lieu of conventional medicine
Alternative medicine is a broad category including herbal dietary supplements, acupuncture, chiropractic, energy therapies and other therapies that are not part of standard conventional (here also called, traditional) Western-based medical care. Many of these alternative therapies have uncertain healing effects although some techniques have been shown to help relieve pain and nausea and are used as complementary treatments in addition to conventional, standard medical care.
About one-third (32%) of U.S. adults say they have heard a lot about alternative medicine, and 54% say they have heard a little, while 13% say they have heard nothing at all about alternative medicine.
About half of the general public reports that they have tried alternative medicine either instead of (20%) or in conjunction with (29%) conventional medical treatments. Half of U.S. adults say they have never used alternative medicine.
Older adults, ages 65 and older, are a bit less likely than younger age groups to have used alternative medicine instead of conventional treatment (10% have done so compared with 22% each of those ages 18-49 and 50-64).
There are no significant differences by gender or education in having tried alternative medicine in lieu of conventional health care.7
The National Health Interview Survey conducted by the Centers for Disease Control and Prevention found that people with chronic conditions use more complementary and alternative medical treatments.8 The Pew Research Center survey also finds people who report having a chronic medical condition are more likely to have used alternative medicine in addition to traditional medicine (33% have done so compared with 24% of those who do not have a chronic condition or disease).
About one-in-twelve Americans report that they never use over-the-counter medications
Overall, most Americans report that they use over-the-counter medications either right away (41%) when experiencing cold or flu symptoms or that they do so after symptoms worsen (49%). Some 8% of Americans say they never take over-the-counter medications.
No single demographic or educational group stands out as never taking over-the-counter medications for cold and flu symptoms. However, those who say this are more likely than other Americans to have tried alternative medicine instead of conventional treatment.
Roughly one-third (34%) of people who say they never take over-the-counter medications say they have tried alternative medicine instead of conventional medical care. By comparison, 18% of those who say they take over-the-counter medications right away have used alternative medicine instead of a conventional treatment.
Preventive health care behaviors correlate with people’s use of conventional and alternative medicine
Preventive health care aims to promote health and well-being through regular checkups, immunizations and screening tests. Roughly three-quarters of Americans (76%) say they have a primary care provider. Some 69% of Americans say that they have gone to a health care provider for a physical examination in the past year, and 40% say they have had a flu shot in the past year.
Americans’ habits toward using conventional medicine are associated with their preventive health care behaviors. For example, among the minority of Americans who say they never take over-the-counter medications for cold and flu symptoms, fewer have a primary care provider (65% compared with 80% of those who take over-the-counter medications right away), had a physical exam in the past year (61% vs. 74% of those who take over-the-counter medications right away) or had a flu shot in the past year (20% vs. 45% of those who take over-the-counter medications right away).
Those who have used alternative medicine instead of conventional treatment are also slightly less likely to have a primary care provider or to have had a preventive care checkup or flu shot in the past year.
About three-in-ten Americans say they supplement a health care provider’s advice in order to check for other options or to learn about potential side effects of recommended treatments
When it comes to making decisions about treatment for a serious health problem, three-in-ten Americans (30%) say they just ask a doctor for advice. Roughly two-thirds of the public (68%) says they ask a health care provider for advice and also do their own research, either to check for other treatments (21% of U.S. adults), to understand potential side effects for a recommended treatment (9%) or simply to learn more about the recommended treatment (36%).
Americans who report never taking over-the-counter medications for cold and flu symptoms are more likely to say that they do their own research to check for other treatment options than do people who take such medications at the first sign of symptoms. Some 36% of those who never take over-the-counter medications say they do their own research in order to check for other treatments, compared with 17% of those who take over-the-counter medications right away.
People who have tried alternative medicine are a bit more likely than other Americans to say they supplement a doctor’s advice with their own research, especially to check for other treatment options.
Public Opinion about Childhood Vaccines for Measles, Mumps, and Rubella
Public debate over the safety of childhood vaccines, particularly the vaccine for measles, mumps and rubella, is typically linked with a 1998 research study – later discredited – that suggested that the MMR vaccine was associated with autism.9 Seth Mnookin’s book, The Panic Virus, suggests that media reporting of the study coupled with the 12 years it took until the study was retracted helped foster concerns about the safety of the MMR vaccine among, at least, some members of the public. And Dina Fine Maron suggests that the coincidental discovery of many neurological disorders around the age of 2 contributes to ongoing concerns about vaccines, especially among parents of young children.
A number of prominent public figures have expressed reservations about the safety of childhood vaccines, especially the MMR vaccine, which is recommended to be given to children between the ages of 12 and 15 months, followed by a second dose at the age of 4 to 6 years. For example, actor Robert De Niro selected a film for the Tribeca Film Festival that argued for a link between childhood vaccines and autism. The film was later dropped from the festival in response to protests, but De Niro, who has an autistic son, repeated his personal concerns about the safety of vaccines and urged people to see the film. A number of political figures have raised concerns about the safety of childhood vaccines. President Trump questioned the recommended schedule for childhood vaccines during a primary debate in 2015, met with members of the anti-vaccine movement during the 2016 campaign and as president-elect, reportedly asked Robert Kennedy Jr., the editor of a volume that argues the preservative used in some vaccines causes autism and other neurological disorders, to head a commission on vaccine safety.
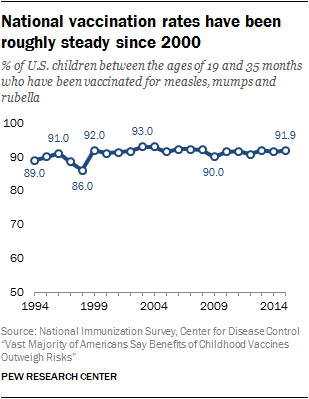
Roughly nine-in-ten children receive the first dose of the measles, mumps and rubella vaccine by the age of 35 months. In 2014, 91.9 percent of children ages 19 to 35 months had received the MMR vaccine, according to data from the Centers for Disease Control and Prevention.
However, local vaccination rates can vary widely. A preliminary analysis published in JAMA Pediatrics suggested that the “substandard” vaccination rates – that is, vaccine rates below the level needed to protect the population from the measles disease – were likely to blame for the outbreak of measles originating at Disneyland in December 2014 and continuing through the early months of 2015.
The new Pew Research Center survey finds that a large majority of Americans consider the preventive benefits of the MMR vaccine to be high and the risk of side effects from the MMR vaccine to be low. Overall, some 88% of Americans think the benefits of the MMR vaccine outweigh the risks; just one-in-ten dissent from this view.
Pockets of Americans appear more hesitant about the safety of vaccines, however. Parents of younger children (from birth to age 4) tend to rate the risk of side effects from the MMR vaccine as higher and the benefits lower than parents with older children and those with no minor-age children. Blacks are more likely than whites to think there is either a medium or high risk of side effects from the MMR vaccine. And people with less knowledge about science and those with lower levels of education and family income also express comparatively more concern about the risk of side effects from the MMR vaccine. On the flip side, people with high knowledge about science, higher education and higher family income levels are comparatively more inclined to see high health benefits from the MMR vaccine.
In addition, people’s conventional and alternative medicine practices tend to align with their perceptions of the risks and benefits of the vaccine. The minority of Americans who report never using over-the-counter medications for cold and flu symptoms, for example, are especially likely to see medium or high risk from the MMR vaccine. Similarly, those who have used alternative medicine instead of conventional treatment are more inclined to think the risk of side effects from the vaccine is medium or high.
When it comes to policy views, a large majority of Americans support school-based requirements for the MMR vaccine in order to protect public health; fewer than two-in-ten think parents should be able to choose whether or not to have their children vaccinated for measles, mumps and rubella.
Older adults, especially those ages 65 and older, and those with high science knowledge are particularly strong in their support for school-based policy requirements to vaccinate children for measles, mumps and rubella. Reports that affluent communities have lower vaccination rates lead some to speculate that people with higher incomes are particularly concerned about the safety of the MMR vaccine. The survey finds, however, that people with higher family incomes see low risk of side effects from the MMR vaccine and are especially strong in their support for a requirement that all children be vaccinated against MMR in order to attend public schools.
White evangelical Protestants are slightly more likely than either white mainline Protestants or Catholics to think that parents should able to decide not to have their children vaccinated, even if that may create health risks for other children and adults. And, political conservatives, regardless of party affiliation, are more likely than either moderates or liberals to support parents being able to choose whether to have their children vaccinated. Majorities of white evangelical Protestants and political conservatives, however, support a school-based requirement for the MMR vaccine.
Smaller majorities of people who say they never take over-the-counter medications for cold and flu symptoms and those who have used alternative medicine instead of conventional treatment support school-based requirements for the MMR vaccine; comparatively more in these groups say that parents should be able to decide whether their children should be vaccinated for MMR even if that decision creates health risks for others.
Personal concern about childhood vaccine issues
Some 42% of Americans say that they care “a great deal” about issues related to childhood vaccines. An additional 39% say they care “some,” while a small share, 17%, say they care not too much or not at all about these issues.
Women are more likely than men to be deeply concerned about childhood vaccine issues (48% of women vs. 36% of men care a great deal about these issues). A larger share of blacks (61%) than either Hispanics (43%) or whites (37%) report caring a great deal about childhood vaccine issues.
About half (49%) of parents with young children (up to age 4) care deeply about childhood vaccine issues, as do 40% of those who do not have minor-age children.
There are no differences in level of concern between mothers and fathers of minor-age children or across education or income levels.
There are no more than modest differences in beliefs about the benefits and risks of the MMR vaccine by levels of concern about childhood vaccine issues.
A large majority of Americans see benefits from childhood vaccines, but several subgroups show comparatively more concern about vaccine risks
Most Americans rate the preventive health benefits of childhood vaccines for measles, mumps and rubella as high and the risk of side effects as low. Fully 73% of U.S. adults say the health benefits of the MMR vaccine are high, while a quarter of adults say the benefits are medium (18%) or low (7%). On the flip side, most Americans consider the risk of side effects from the MMR vaccine to be low (66%), 21% say the risks are medium and 11% say the risks are high.10
When asked to weigh the risks and benefits of childhood vaccines together, an overwhelming majority of Americans say the benefits of childhood vaccines outweigh the risks (88%), and only one-in-ten say the risks outweigh the benefits.
Those high in science knowledge are especially likely to see health benefits from the MMR vaccine; fewer parents of young children, young adults and blacks perceive high benefits
While most Americans are in agreement that childhood vaccines for measles, mumps and rubella have high preventive health benefits and a low risk of side effects, there are notable differences in views among subgroups. People with more science knowledge (as well as those with higher levels of education) are especially inclined to see benefits from the MMR vaccine.11
Parents of young children along with blacks are less inclined to see benefits and comparatively more inclined to say the risk of side effects of the MMR vaccine is medium or high.
For example, fully 91% of those with high science knowledge rate the preventive health benefits as high, compared with 55% of those with low science knowledge. By the same token, 19% of those with high science knowledge rate the risk of side effects from the MMR vaccine as medium or high, compared with 47% of those with low science knowledge. A similar pattern occurs by education; people with a postgraduate degree are more inclined than those with a high school diploma or less to see the health benefits of the MMR vaccine as high and the risks of side effects as at least medium.
People with lower family incomes are more inclined than people whose family income is at least $50,000 per year to see risks from the MMR vaccine and less inclined to see preventive health benefits.
Some 79% of whites say that preventive health benefits of childhood vaccines for MMR are high, compared with 56% of blacks and 61% of Hispanics.12 Blacks (44%) are also more likely than either whites (30%) or Hispanics (33%) to say the risk of side effects from the MMR vaccine is medium or high.
Parents of children ages 0 to 4, a group that tends to skew younger than the population as a whole, are less inclined than other adults to believe that the preventive health benefits of childhood vaccines are high (60% vs. 75% of those with only older children and 76% of those without minor-age children). Parents with children under age 4 are relatively more likely to say the risk of side effects from the MMR vaccine is medium or high (43% vs. 29% of those with no minor-age children).
There are no more than modest differences between men and women in perceptions of benefit and risk from the MMR vaccine.
Majorities of all major religious groups rate the preventive health benefits as high, and minorities rate the risk of side effects from the MMR vaccine as high or medium. Black Protestants, like blacks in general, are less likely to consider the preventive benefits of the measles, mumps and rubella vaccine to be high and more inclined to see the risk of side effects from such a vaccine as medium or high. Other religious groups tend to give similar assessments of the benefits and risks from the MMR vaccine.
When people give their overall judgment of the trade-offs, fully 88% of Americans say the benefits of childhood vaccines for measles, mumps and rubella outweigh the risks, just one-in-ten (10%) say otherwise.
There are modest differences by science knowledge, parent status, age, race and ethnicity. People with high (93%) or medium (90%) science knowledge are more likely than those with low science knowledge (81%) to think the benefits of the MMR vaccine outweigh the risks. Whites (92%) are more inclined than blacks (82%) and Hispanics (78%) to say the benefits of childhood vaccines outweigh the risks.
Some 81% of parents with children ages 0 to 4 say the preventive health benefits of the MMR vaccine outweigh the risks, compared with 90% of those with no children under age 18. Similarly, younger adults, ages 18-29, are somewhat less likely than older age groups to consider the benefits of vaccines to outweigh the risks (79% compared with at least 90% of those in older age groups.)
Statistical models underscore the strong relationship between people’s level of science knowledge, their age and their parent status in predicting their beliefs about the MMR vaccine. There are also modest race differences when it comes to views on the preventive health benefits of the MMR vaccine even after controlling for other factors.
People’s medical care practices are also linked to their beliefs about the MMR vaccine
People’s practices regarding conventional and alternative medicine are also associated with their views about childhood vaccines. In particular, those who never take over-the counter medication and people who have used alternative medicine instead of conventional medical treatment perceive higher risks from the MMR vaccine, compared with other Americans.
Some 49% of people who say they never take over-the-counter medications consider the risk of side effects from the MMR vaccine to be medium or high. By comparison, 33% of those who take over-the counter medications for cold and flu symptoms right away say the same. Those who never take over-the-counter medications are also less likely to rate the preventive health benefits of the MMR vaccine as high (59% do so vs. 73% among those who take over-the-counter medications right away).
Similarly, people who have used alternative medicine instead of traditional, Western-based medical treatment are somewhat more likely to see a higher risk of side effects from the MMR vaccine. Some 42% of this group says the risks of the MMR vaccine are medium or high, compared with three-in-ten (30%) among those who have never used alternative medicine. Ratings of benefits from the MMR vaccine are roughly the same across these groups.
When Americans weigh the benefits and risks of childhood vaccines, similar patterns emerge. While an overwhelming majority of all subgroups say the benefits of the MMR vaccine outweigh the risks, people who never take over-the-counter medications are slightly more inclined to think the risks outweigh the benefits. Some 74% of those who report never taking over-the-counter medications say the benefits outweigh the risks, 23% of this group says the risks predominate. In contrast, nearly all of those who take over-the-counter medications for cold or flu symptoms right away say the benefits of the MMR vaccine outweigh the risks (91% vs. 7%).
Summary judgments of the risk-benefit trade-offs are about the same regardless of experience with alternative medicine.
Statistical models find people’s practices regarding over-the-counter medications and alternative medicine are significantly associated with perceived risk from childhood vaccines when controlling for demographic and other factors.
Perceived safety of childhood vaccines in 2015 survey linked with age, education
A Pew Research Center survey conducted in 2015 shortly after an outbreak of measles, found a large majority (83%) of Americans thought childhood vaccines, such as MMR, were generally safe for healthy children, while only 9% believed childhood vaccines were not safe. Older adults and those with more education were a bit more likely to consider vaccines safe. Fully 91% of those ages 65 and older said vaccines were safe for healthy children; by comparison, 77% of those ages 18 to 29 said vaccines were safe. Roughly nine-in-ten (92%) college graduates said childhood vaccines were safe for healthy children. Smaller majorities of those with some college (85%) or a high school diploma or less (77%) said vaccines were generally safe.
More than eight-in-ten Americans favor school-based vaccine requirements; a minority says vaccines should be parents’ choice
A majority of the American public (82%) says the measles, mumps and rubella vaccine should be a requirement “in order to attend public schools because of the potential risk for others when children are not vaccinated.” Some 17% of Americans believe that “parents should be able to decide not to vaccinate their children, even if that may create health risks for other children and adults.”
Majorities of Americans across a range of demographic and educational groups support school requirements for the MMR vaccine. Older adults are especially strong in their support. Fully nine-in-ten (90%) adults ages 65 and older favor a school-based requirement that children be vaccinated for measles, mumps and rubella. A smaller majority of younger age groups say the same (77% of adults ages 18-29 and 78% of adults ages 30-49).
Parents of younger children, school-age children and those with no minor-age children hold roughly similar views on this issue with a majority of all three groups saying that healthy schoolchildren should be required to be vaccinated because of the health risk to others when children are not vaccinated.
People who care a great deal about childhood vaccine issues are more inclined to support school-based MMR vaccine requirements (87% favor this, compared with 80% of those who care some about childhood vaccine issues and 78% of those who care not too much or not at all about childhood vaccine issues).
On average, people with higher family incomes, earning at least $100,000 annually, are a bit more inclined than those with lower incomes to support requiring the MMR vaccine for all public schoolchildren.
Views about this issue are about the same by political party. However, political conservatives are more likely than either moderates or liberals to say that parents should be able to decide not to have their children vaccinated, even if that decision creates health risks for others.
White evangelical Protestants (22%) and the religiously unaffiliated (21%) are slightly more likely than white mainline Protestants and Catholics to say parents should be able to decide not to have their children vaccinated, even if that may create health risks for other children and adults. However, as noted above, the major religious groups have roughly similar views of the risks and benefits from the MMR vaccine.
The survey found no or only small differences by gender, race and education on this issue.
Statistical models show that, on average, adults ages 65 and older are more likely than younger age groups to support school-based MMR vaccine requirements when controlling for demographic and other factors. In addition, conservatives are more likely than either moderates or liberals to say that parents should be able to decide whether to have their children vaccinated. Evangelical Protestants (of any race) are more likely than mainline Protestants to say that parents should be able to decide whether to have their children vaccinated even if it creates a health risk for others, when statistically controlling for other factors.
Public views on requiring vaccines in 2014 survey also differed by age, religion
A 2014 Pew Research Center survey asked a more general question about vaccines. In that survey, 68% of U.S. adults said children should be required to be vaccinated for childhood diseases such as measles, mumps, rubella and polio, while 30% said parents should be able to decide whether to have their children vaccinated. Adults younger than 30 were less inclined than those ages 65 and older to think such vaccines should be required (59% of those ages 18 to 29, compared with 79% of those ages 65 and older). White evangelical Protestants were comparatively less inclined to favor requiring childhood vaccines (59%). By comparison, 70% of white mainline Protestants and 76% of Catholics supported requiring childhood vaccines. Views on this issue were slightly different by party; 64% of Republicans and leaning Republicans said vaccines should be required, compared with 74% of Democrats and leaning Democrats.
People’s practices in using conventional and alternative medicine are linked with their beliefs about school requirements for the measles, mumps and rubella vaccine
People who never take over-the-counter medication for cold or flu symptoms and people who have used alternative medicine instead of conventional treatment are more likely than other Americans to say parents should be able to decide whether to have their children vaccinated, even if not vaccinating them may create health risks for other people.
A third (33%) of people who never take over-the-counter medications say that parents should be able to decide whether to have their children vaccinated; two-thirds (66%) of this group say that children should be required to be vaccinated in order to attend public school. In contrast, just 12% of those who take over-the-counter medications right away say that parents should be able to decide whether to have their children vaccinated for measles, mumps and rubella; 86% say children should be required to be vaccinated in order to attend school.
Similarly, people who have used alternative medicine instead of traditional medicine are a bit more inclined (26% compared with 13% of those who have never tried alternative medicine) to think parents should be able to decide whether to have their children vaccinated, though the majority support a school-based requirement for the MMR vaccine.
Statistical models find that people’s practices regarding over-the-counter medications and alternative medicine are significantly associated with support for school-based MMR vaccine requirements. On average, those who never take over-the-counter medications for cold or flu symptoms and those who have used alternative medicine instead of conventional medicine are more likely to say that parents should be able to decide whether to have their children vaccinated, when controlling for demographic and other factors.
Public Trust in Medical Scientists and Their Research on Childhood Vaccines
Public trust in information from medical scientists about the health effects of the measles, mumps and rubella vaccine is more positive than negative. And more Americans trust information about this topic from medical scientists than from pharmaceutical industry leaders, people from holistic or alternative health groups, the news media or elected officials.
Most Americans see broad consensus among medical scientists that the MMR vaccine is safe for healthy children. Public perceptions of medical scientists’ understanding about the vaccine also tilt positive. Nearly half of Americans think medical scientists understand the health risks and benefits of such vaccines very well, while a nearly equal portion rate their understanding as “fairly well”; only a small minority says medical scientists do not understand the health effects of the MMR vaccine at all or not too much.
About half or more Americans have a positive view of medical research about vaccine safety, saying that the best interests of children’s health and the best available scientific evidence influence research most of the time. By comparison, fewer people say that researchers’ desire to help connected industries or advance their careers influence medical research on vaccines most of the time.
There is considerable variation in public views about medical scientists, however. People with high knowledge about science, based on an index of nine general science questions, have more positive views of medical scientists and their research on vaccines than do those with low science knowledge. There is a similar, though less pronounced, tendency for people who care more deeply about childhood vaccine issues to see medical scientists in a more positive light.
There are modest differences in trust by generation, with younger adults a bit more skeptical than older generations about medical scientists and their research. Statistical models show that seniors, ages 65 and older, are consistently more likely than those ages 18 to 29 to hold positive views of medical scientists and their research on childhood vaccines, when controlling for demographic, education and political factors.
Overall, though, a strong majority of Americans support a role for medical scientists in policy decisions related to childhood vaccines.
Roughly half of Americans say almost all medical scientists are in agreement that vaccines are safe and that medical scientists understand the effects of childhood vaccines very well
Some 55% of the general public says that “almost all” medical scientists see childhood vaccines for measles, mumps and rubella as safe for healthy children. An additional 28% say more than half of medical scientists are in agreement on this, while 15% say that about half or fewer medical scientists think that childhood vaccines are safe for healthy children.
A number of medical and scientific associations have issued statements about the safety of childhood vaccines, although most do not characterize the beliefs of medical scientists. A consensus study from National Academies of Sciences, Engineering and Medicine in 2011 reviewed the evidence for adverse effects connected with all vaccines recommended by the Centers for Disease Control and Prevention for routine administration in children including the MMR.13 It concluded “the MMR vaccine is linked to a disease called measles inclusion body encephalitis, which in very rare cases can affect people whose immune systems are compromised” and rejected a relationship between the MMR vaccine and autism.
A 2014 survey by the Pew Research Center found that 86% of U.S.-based members of the American Association for the Advancement of Science (AAAS) (and 87% of members who are working Ph.D. biomedical scientists) said that childhood vaccines such as the MMR and polio vaccines should be required. Just 13% said that the decision about whether to get vaccinated should be left to parents.
Nearly half of Americans (47%) think medical scientists understand the health risks and benefits of childhood vaccines very well, and 43% say medical scientists understand the risks and benefits fairly well. Just one-in-ten (10%) Americans think medical scientists understand the health risks and benefits not too well or not at all well.
Roughly half of U.S. adults trust medical scientists a lot for information about the effects of vaccines; trust in information from other groups is much lower
Some 55% of Americans say that they trust medical scientists a lot to give full and accurate information about the risks and benefits of childhood vaccines. An additional 35% trust medical scientists at least some, and just 9% say they do not trust information from medical scientists about the risks and benefits at all or not too much.
Trust in information from other groups is much lower, by comparison. Just 13% of Americans trust information from pharmaceutical industry leaders a lot. At the same time, just 9% of Americans trust information on the effects of the MMR vaccine a lot from holistic or alternative health groups.
Few people have a lot of trust in information from either the news media (8%) or elected officials (6%) about the health effects of the MMR vaccine; fully 56% of Americans say they do not trust media information on this at all or not too much, and 67% say the same about information from elected officials.
Roughly half of Americans say medical research is influenced by the best available scientific evidence and concern for children’s health most of the time
Many Americans have a positive view of medical research about vaccine safety; roughly half say such research reflects the best interests of children’s health (55%) and the best available scientific evidence (52%) most of time.
Smaller shares of the public say such research is influenced by medical scientists’ desire to help their industries (27%), their desire to advance their careers (27%) or their own political leanings (18%) most of the time.
Patterns in public trust of medical scientists and vaccine research
Those with more knowledge about science, in general, are especially likely to see consensus among medical scientists about the safety of the measles, mumps and rubella vaccine and to trust information from medical scientists about the effects of the MMR vaccine.
Eight-in-ten adults with high science knowledge (80%) say that almost all medical scientists consider the MMR vaccine to be safe. In contrast, 43% of those with low science knowledge think almost all medical scientists agree on this. Similarly, those with high science knowledge are more likely that those with low science knowledge to think medical scientists understand the health risks and benefits of the MMR vaccine very well (64% vs. 37%).
People with high science knowledge are more trusting of information from medical scientists. Some 73% of this group says they trust medical scientists a lot to give full and accurate information about the health effects of the MMR vaccine, compared with 40% of those with low science knowledge.
People high in science knowledge are more inclined to see medical research on vaccines in a positive light. Seven-in-ten (70%) of them say medical research is influenced by concern for the best interests of children’s health most of the time, compared with 43% of those low in science knowledge. Fully 72% of those high in science knowledge say childhood vaccine research is influenced by the best available scientific evidence most of the time, compared with 34% of those low in science knowledge.
People’s science knowledge levels are closely associated with education. There are similar differences across educational groups in views about medical scientists and their research on childhood vaccines.
And, there is similar tendency, though a bit less pronounced, for those with a deep concern about childhood vaccine issues to express more trust in medical scientists and their research compared with those who do not care at all or not too much about these issues.
There are differences by age in views about medical scientists and their research. Younger adults, ages 18 to 29, are a bit less likely than older age groups to say that medical scientists understand the health effects of childhood vaccines very well and to perceive strong consensus among medical scientists about the safety of the MMR vaccine.
Compared with older adults, those ages 18 to 29 are somewhat less likely to think the best available evidence influences research findings on childhood vaccines most of the time.
Trust in information from medical scientists is roughly the same across age groups, though a somewhat larger share of adults ages 18 to 29 do not trust information about the effects of vaccines from medical scientists at all or not too much.
There are modest differences in views of medical scientists connected with people’s use of alternative and conventional medicine. People who have used alternative medicine instead of conventional treatment are a bit less likely to see medical scientists as understanding the health risks and benefits of the MMR vaccine very well (38% compared with 47% of those who have never tried alternative medicine).
People who have used alternative medicine instead of traditional medicine are less trusting of information from medical scientists (43% trust medical scientists a lot vs. 59% of those who have never used alternative medicine). But even among those who have tried alternative medicine, few say they trust information from people in holistic or alternative health groups a lot to give full and accurate information about the health effects of the MMR vaccine. And views about the influences on medical research related to childhood vaccines are about the same or only slightly different depending on one’s past use of alternative medicine.
Similarly, the 8% of Americans who say they never take over-the-counter medications for cold and flu symptoms are less likely than other Americans to believe that medical scientists understand the risks and benefits of the MMR vaccine very well (33% do so compared with 48% of those who take such medications right away). Those who never take over-the-counter medications are also less likely to trust information from medical scientists; some 34% of this group does not trust information from medical scientists at all or not too much, compared with 5% of those who take these medications right away. They are about equally likely to think the best available evidence influences medical research most of the time (44% vs. 49% of those who take these medications right away). However, differences in views about medical scientists and their research by use of over-the-counter medications or alternative medicine have no more than modest effects in statistical models when demographic and other factors are statistically controlled.
Overall, statistical models show that people with higher levels of science knowledge and greater concern about childhood vaccine issues are consistently associated with more positive views of medical scientists, even when statistically controlling for demographics, education and political factors. In addition, adults ages 65 and older are consistently more likely than younger adults to hold positive views of medical scientists across this set of measures in statistical models controlling for demographic and other factors.
Views about medical scientists and their research on childhood vaccines are roughly the same across racial and ethnic groups, though beliefs about the risks and benefits of vaccines vary across these groups.
There are modest religious group differences in public trust in medical scientists on some of these measures. For example, white evangelical Protestants are less likely to trust information from medical scientists about the effects of the MMR vaccine compared with white mainline Protestants, Catholics and the religiously unaffiliated. White evangelical Protestants rate medical scientists’ understanding of the risks and benefits of the MMR vaccine lower than do either white Catholics or the religiously unaffiliated. And, white evangelical Protestants are less likely than either white Catholics or the religiously unaffiliated to think medical research on childhood vaccines is influenced by the best available scientific evidence most of the time. A separate series of statistical models, not shown in this report, find differences by religious affiliation on these three judgments are statistically significant even when controlling for demographics, education and political factors.
Most Americans support a major role for medical scientists in policymaking on childhood vaccine issues
Some 73% of U.S. adults say medical scientists should play a major role in policymaking decisions related to childhood vaccines. A smaller share, 47%, says the general public should play a major role in policy decisions about childhood vaccines.
A minority of Americans say pharmaceutical industry leaders (27%), health insurance company leaders (26%) and elected officials (25%) should have a major role in policy decisions on childhood vaccine issues.
Public Views of Media Coverage on Childhood Vaccines
Most Americans say the media are doing a good job reporting issues related to childhood vaccines. People who care deeply about childhood vaccine issues and those who follow such news reports more closely are especially positive in their views of news coverage on this topic. Young adults, ages 18 to 29, are more negative in their overall views of media coverage.
Half of Americans say they follow news about childhood vaccines at least somewhat closely, with 13% saying they follow very closely and 37% somewhat closely.
Those who care a great deal about childhood vaccine issues and parents of young children are much more likely to follow such news closely. Fully 76% of Americans who say that they care “a great deal” about issues related to childhood vaccines say they follow news regarding the topic very or somewhat closely, compared with 38% of those who care some and 17% of those who do not care at all or not too much about these issues.
Parents of children through age 4 are especially likely to follow news about childhood vaccines closely; 26% of this group say they follow news reports on the topic very closely. This compares with 9% of parents with school-age children only (ages 5-17).
Blacks, women and adults ages 65 and older adults are especially likely to follow news about childhood vaccines somewhat or very closely.
Overall, a 61% majority of Americans say the media are doing a good job reporting on issues related to childhood vaccines for measles, mumps and rubella; 37% say they are doing a bad job.
People who follow vaccine news reports more closely are particularly positive about media coverage on the MMR vaccine; 73% of this group say the media do a good job, compared with 50% of those who do not follow such news reports at all or not too closely.
People who care a great deal about childhood vaccine issues are also more positive in their views of media coverage. About seven-in-ten (69%) of those who care a great deal about vaccine issues say the media do a good job covering the MMR vaccine. This compares with 46% of those who do not care too much or at all about childhood vaccine issues.
Parents with young children (ages 0 to 4) hold roughly similar views as other Americans on media performance in covering MMR vaccine issues.
Blacks, adults age 65 and older, and Democrats have more favorable views of media coverage on the MMR vaccine.
Fully 83% of blacks say that the news media do a good job covering MMR vaccine issues, compared with 55% of whites and 65% of Hispanics.
Some 75% of adults ages 65 and older say the news media are doing a good job covering MMR vaccine issues compared with 41% of adults ages 18-29.
More Democrats (70%) than Republicans (52%) say the media are doing a good job covering issues about the MMR vaccine.
On balance, more Americans say media coverage on these issues generally exaggerates the health risks of childhood vaccines (39%) than say the media do not take the health risks seriously enough (24%). A third of adults (33%) say the media are about right in their reporting on these issues.
Similarly, four-in-ten adults (40%) say that the media generally give too much attention to skeptics of vaccines, while 24% say the media give too little attention to skeptics of vaccines. About a third (32%) of Americans say media reporting gives about the right amount of attention to skeptics of vaccines.
Men, whites, adults ages 18 to 49 and those with higher levels of science knowledge are slightly more likely to say that the news media exaggerate the health risks of childhood vaccines. These groups are also slightly more likely to see news coverage as giving too much attention to skeptics of vaccines.
Notes
- Kennedy, Robert Jr., ed., 2014. Thimerosal: Let the Science Speak: The Evidence Supporting the Immediate Removal of Mercury-—a Known Neurotoxin-—from Vaccines. New York: Skyhorse Publishing.
- We asked nine questions of respondents to assess their level of broad knowledge about science. The questions in the nine-item index of science knowledge are shown in the survey questionnaire and topline. Some 22% of respondents are classified as high in science knowledge, 48% are medium and 30% are classified as low in science knowledge. More details are available in Chapter 4 and the Methodology section of the related report, “The Politics of Climate.”
- Past public surveys have used a number of different definitions and approaches to measuring people’s use of alternative medicine. See P.E. Harris, K.L. Cooper, C. Relton and K.J. Thomas, 2012. Prevalence of complementary and alternative medicine (CAM) use by the general population: A systematic review and update. International Journal of Clinical Practice, vol. 66 (10): 924-939.
- The sample of Hispanics in this survey is predominantly U.S. born and English-dominant.
- These findings are in keeping with a 2014 Pew Research Center survey which found older adults more likely than younger adults to have an interest in health and medicine topics, generally.
- Schoenfeld, J.D. and Ioannidis, J.P. 2012. Is everything we eat associated with cancer? A systematic cookbook review, The American Journal of Clinical Nutrition, 97(1): 127-134.
- Other research has found that women and more highly educated adults are more likely to use complementary and alternative medicine. There are wide differences in definitions and question wording in surveys about alternative medicine, however, that could account for such differences. See Harris, P.E., Cooper, K.L., Relton, C. and Thomas, K.J. 2012. Prevalence of complementary and alternative medicine (CAM) use by the general population: A systematic review and update. International Journal of Clinical Practice, vol. 66 (10): 924-939.
- Falci, L., Shi, Z., Greenlee, H. 2016. Multiple chronic conditions and use of complementary and alternative medicine among US adults: Results from the 2012 National Health Interview Survey. Preventing Chronic Disease, vol. 13: 150501.
- See Public Trust in Vaccines: Defining a Research Agenda, 2014. American Academy of Arts & Sciences.
- Responses of very high/high and very low/low are combined. See questionnaire wording and topline.
- The questions in the nine-item index of science knowledge are shown in the survey questionnaire and topline. More details are available in in Chapter 4 and the Methodology section of the related report, “The Politics of Climate.”
- The sample of Hispanics in this survey is predominantly U.S. born and English-dominant.
Originally published by Pew Research Center with permission.