

Functional medicine’s vocabulary is dressed in scientific language. But language is not substance.

By Matthew A. McIntosh
Public Historian
Brewminate
Introduction
In the sprawling marketplace of modern health trends, functional medicine has emerged as a popular—yet deeply controversial—movement. Promising to treat “root causes” rather than symptoms, it bills itself as an evolution beyond conventional medicine. However, beneath its appealing rhetoric lies a system built more on anecdote than evidence, heavily reliant on pseudoscientific diagnostics and therapies that often do more harm than good.
What masquerades as holistic or “integrative” care is, in truth, a repackaging of disproven ideas under the imprimatur of scientific-sounding jargon. Functional medicine has not only failed to meet the rigorous standards of peer-reviewed science but has also increasingly endangered patients by leading them away from effective, evidence-based treatments.
Origins of a Modern Movement
Functional medicine was formalized in the 1990s by biochemist Jeffrey Bland, who envisioned it as a personalized, systems-based approach to healing. It claims to examine the interactions between genetics, environment, and lifestyle that might influence long-term health. On its face, this ambition sounds admirable, even aligned with emerging fields like epigenetics or personalized medicine.
Yet, functional medicine strays quickly from scientific moorings. Its primary institutions, such as the Institute for Functional Medicine (IFM), offer seminars and certifications in tests and treatments that lack support from mainstream clinical research.1 Medical schools do not teach functional medicine. It is not recognized by the American Board of Medical Specialties. Still, its practitioners often use the MD title and the aesthetics of clinical practice to build credibility and charge premium fees.
A House Built on Faulty Tests
One of the most egregious features of functional medicine is its widespread use of unvalidated diagnostic tests. Patients are routinely subjected to expensive lab work for “adrenal fatigue,” “leaky gut syndrome,” “toxin overload,” “chronic candidiasis,” and other conditions that have been debunked or dismissed by the broader medical community.2
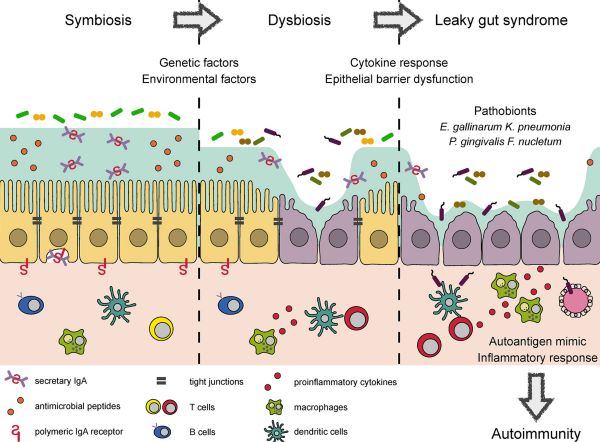
Take adrenal fatigue, for example. This supposed condition posits that chronic stress wears out the adrenal glands, causing fatigue, weight gain, and brain fog. Yet according to the Endocrine Society, adrenal fatigue is a myth: cortisol levels in sufferers are often normal, and no credible evidence supports adrenal gland exhaustion in this manner.3 Similarly, leaky gut syndrome is described in vague and variable terms—blamed for everything from acne to arthritis—without consistent diagnostic criteria or reproducible data.4
These diagnostic fictions open the door to treatment fictions. Based on dubious test results, patients are prescribed restrictive diets, unregulated supplements, chelation therapy, and even colon cleanses. Some practitioners advise discontinuing lifesaving medications. In extreme cases, patients are convinced to forego chemotherapy or insulin therapy for “natural” alternatives.5
The Seduction of the “Root Cause”
At the heart of functional medicine is a rhetorical seduction: the idea that conventional doctors merely treat symptoms while functional medicine seeks to uncover the “root cause.” This binary is false and manipulative. Good medicine always seeks underlying causes—be it bacterial infections, endocrine disorders, genetic mutations, or environmental exposures.
What functional medicine does is replace genuine pathophysiology with metaphor. It invents root causes where none exist or repackages symptoms into vague and elastic diagnoses that cannot be disproved. The promise of certainty becomes a weapon: patients are given answers rather than truth. And in a healthcare system rife with bureaucratic failures, many find that irresistible.
Patients burned by rushed visits and chronic mismanagement are easy prey. They turn to functional medicine for compassion and continuity. Unfortunately, that trust is too often rewarded with exploitation—emotional, financial, and physiological.6
Institutional Enablement and Financial Incentives
The danger of functional medicine is not confined to fringe naturopaths. It has gained a foothold in elite hospitals and among credentialed professionals. The Cleveland Clinic, for instance, controversially opened a Center for Functional Medicine in 2014, lending institutional legitimacy to practices its own peer departments might consider suspect.7 Financial incentives play a role: patients pay thousands out-of-pocket for consults, supplements, and follow-ups.
This pay-to-play model erodes the boundary between healthcare and commerce. Supplement sales are often bundled into the practice itself, blurring ethical lines and incentivizing overdiagnosis. Functional medicine is a lucrative brand. Like any brand, it thrives on belief rather than evidence.
Risks to Public Health
While proponents of functional medicine paint it as benign or complementary, the risks it poses to public health are real and measurable:
- Delay of proper treatment: Time-sensitive diseases like cancer, autoimmune disorders, and infections may progress untreated while patients explore unproven remedies.
- Psychological harm: Constant testing and speculation can increase anxiety and foster illness anxiety disorder.
- Financial exploitation: Out-of-pocket costs for consultations and supplements can run into thousands of dollars annually with little or no benefit.
- Erosion of trust in science: Functional medicine often traffics in anti-pharmaceutical, anti-vaccine, and anti-establishment narratives, fueling broader public distrust of evidence-based medicine.8
Conclusion: A Pseudoscience by Another Name
Functional medicine’s vocabulary is dressed in scientific language. But language is not substance. When diagnostic categories are vague, tests unvalidated, and therapies unproven, the label of pseudoscience is not an insult—it is an accurate classification.9
In an era when trust in institutions is fragile and disinformation is rampant, pseudosciences like functional medicine do more than waste money: they erode the foundations of public health. The medical community must not only challenge the false claims of functional medicine but also reckon with the failures of conventional care that allowed such a movement to flourish.
Patients deserve better. Not a choice between neglect and pseudoscience, but compassionate, evidence-based medicine grounded in humility, honesty, and truth.
Endnotes
- Institute for Functional Medicine, “What is Functional Medicine?” ifm.org.
- Gorski, David. “Functional Medicine: Pseudoscience Wrapped in a Lab Coat.” Science-Based Medicine, Jan 2020.
- Endocrine Society, “Adrenal Fatigue Does Not Exist,” endocrine.org, 2016.
- Caulfield, Timothy. Is Gwyneth Paltrow Wrong About Everything? Penguin Canada, 2018.
- Atwood IV, Kimball C. “Functional Medicine: New Name for Old Quackery.” Science-Based Medicine, 2009.
- Gorski, David. “Functional Medicine: Integrative Medicine’s Phony Cousin.” Science-Based Medicine, May 2021.
- Cleveland Clinic, “Functional Medicine Clinic,” clevelandclinic.org.
- Caulfield, Timothy. The Cure for Everything. Beacon Press, 2013.
- Novella, Steven. “The Pseudoscientific Claims of Functional Medicine.” Neurologica Blog, 2020.
Originally published by Brewminate, 06.27.2025, under the terms of a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International license.


