
Modern medicine has its fair share of jaw-dropping innovations—robotic surgeries, gene editing, AI diagnostics. But what if one of the most effective treatments out there doesn’t require a lab full of machines or synthetic chemicals? What if the answer is already inside you?
That’s exactly what’s so compelling about platelet rich plasma (PRP) therapy. It’s not a product of science fiction or a last-ditch miracle cure—it’s a relatively simple treatment that uses your body’s own healing tools to help repair injured tissue, reduce inflammation, and improve mobility. And it’s gaining attention for good reason.
In this article, we’ll break down what PRP is, how it works, what it treats, and why it’s becoming such a go-to option for people who want to heal naturally—without long recovery times or invasive procedures.
What Exactly Is PRP?
Let’s start with the basics. PRP stands for platelet-rich plasma, and it’s made from your own blood. Blood has a few key components: red blood cells, white blood cells, platelets, and plasma (which is mostly water and proteins).
Platelets are best known for helping blood clot when you get a cut. But they also carry a treasure trove of growth factors—natural chemicals that help tissue repair itself. PRP takes advantage of this by concentrating the platelets into a small amount of plasma and injecting it into areas that need healing.
Sounds almost too simple, right? That’s the beauty of it. No synthetic drugs, no general anesthesia, no operating room.
How Is PRP Made?
Here’s what the process usually looks like:
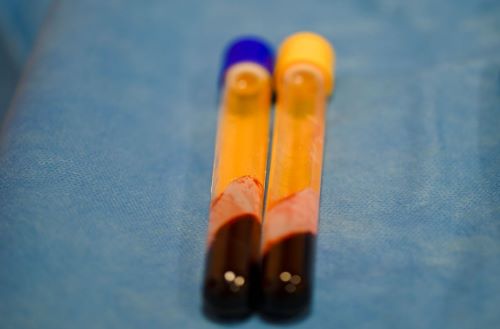
- Blood Draw – A small sample of your blood is taken, just like during a routine lab test.
- Spinning (Centrifugation) – That blood goes into a machine called a centrifuge, which spins it fast enough to separate the components.
- Concentration – The doctor isolates the platelet-rich portion of the plasma.
- Injection – The PRP is then injected into the injured or painful area using imaging guidance (like ultrasound) to ensure accuracy.
The whole process takes about 30 to 60 minutes, and since it’s your own blood, there’s little risk of allergic reaction or rejection.
Why PRP Works So Well
When you injure a ligament, tendon, or joint, your body naturally tries to repair it by sending platelets and other healing factors to the area. The problem is, blood flow to these areas—especially joints—is limited. That slows down healing.
PRP acts like a healing booster shot, delivering a high concentration of platelets directly to the trouble spot. Once there, those platelets release growth factors that:
- Stimulate cell growth
- Boost collagen production
- Reduce inflammation
- Improve blood vessel formation
In plain terms? It gives your body the tools it needs to rebuild tissue and calm pain, faster and more efficiently than it could on its own.
What Conditions Can PRP Treat?
PRP isn’t a magic wand, but it’s surprisingly versatile. It’s especially popular in orthopedic medicine and sports injury clinics. Common conditions treated with PRP include:
Tendinitis and Tendinosis
Tennis elbow, golfer’s elbow, and Achilles tendinopathy are all examples of tendon problems that respond well to PRP.
Osteoarthritis
For people with mild to moderate knee or hip arthritis, PRP can reduce pain and stiffness by improving joint lubrication and slowing cartilage breakdown.
Ligament Injuries
MCL injuries, partial ACL tears, or chronic ankle sprains may all benefit from PRP injections, especially when surgery isn’t needed or wanted.
Rotator Cuff Issues
Shoulder pain from overuse or minor rotator cuff damage can sometimes be improved with PRP therapy.
Muscle Strains
Hamstring and quad strains in athletes often heal faster when PRP is added to rest and rehab.
Some clinics even use PRP for hair loss, skin rejuvenation, and dental surgery—but this article focuses on musculoskeletal uses, where research is strongest.
Who’s Using It? (Hint: It’s Not Just Pro Athletes)
PRP has made headlines thanks to high-profile athletes—Tiger Woods, Rafael Nadal, and Kobe Bryant all used it to return from injuries faster. But it’s not just for elite sports stars anymore.
These days, weekend warriors, middle-aged runners, arthritic seniors, and everyday workers with repetitive stress injuries are turning to PRP to get back on their feet—literally.
That shift is partly thanks to clinics that specialize in regenerative orthopedics, offering PRP as a middle-ground option between physical therapy and surgery. It appeals to people who want results but aren’t ready (or willing) to go under the knife.
What the Science Says (and What It Doesn’t—Yet)
Okay, so does PRP actually work?
The answer is: Yes, for many—but not all—conditions. Research shows promising results, especially for tendinopathies and early-stage osteoarthritis. A few examples:
- A 2021 review in the American Journal of Sports Medicine found PRP significantly outperformed placebo for knee osteoarthritis relief.
- Studies on tennis elbow and plantar fasciitis also show PRP reduces pain and improves function over the long term.
- Some research suggests PRP may even delay the need for joint replacement in mild arthritis cases.
That said, PRP isn’t a guaranteed fix. Results can vary depending on the condition being treated, the severity of the injury, and how the PRP is prepared. Not all PRP is created equal—some clinics use more advanced separation systems or tailor the concentration based on the injury.
PRP vs. Steroid Injections
Steroid injections have long been used to reduce inflammation and pain. They work fast—but only temporarily—and repeated use can actually damage tissue over time.
PRP works slower but promotes healing, not just symptom relief. Think of it like this:
- Steroids: Quick pain relief, but no long-term repair.
- PRP: Slower start, but supports actual recovery.
If you’re dealing with a chronic condition that keeps flaring up, PRP might offer a more sustainable solution.
The Recovery Timeline: What to Expect
One of the best things about PRP is that downtime is minimal. Most people can return to work or light activity within a day or two, though your provider may recommend avoiding intense exercise for a couple of weeks.
Here’s a general idea of what recovery looks like:
- Day 1-3: Some soreness or swelling around the injection site
- Week 1-2: Early healing responses begin
- Week 3-6: Pain often starts improving noticeably
- Month 2-3: Tissue repair continues, with long-term benefits showing up
PRP isn’t an overnight cure, but many people find the results well worth the wait—especially when it helps them avoid surgery.
Is PRP Covered by Insurance?
In most cases, no. PRP is still considered “investigational” by many insurance companies, which means it’s often paid out of pocket. Costs range from $500 to $2,000 depending on the clinic, location, and number of injections.
That may sound steep, but compared to surgery or long-term medication costs, many patients see it as a worthwhile investment—especially if it keeps them moving and out of the OR.
Who Shouldn’t Get PRP?
PRP is generally very safe, but it’s not for everyone. People with the following conditions may be advised to skip it:
- Blood disorders or clotting issues
- Active infection
- Certain types of cancer
- Low platelet count
- Pregnancy (in some cases)
Always talk to a qualified medical provider who understands PRP therapy and your specific health history.

Final Thoughts: A Natural Way to Get Back to Life
The idea that something as simple as your own blood could help heal a stubborn injury sounds almost too good to be true—but PRP proves that the body has more healing power than we often give it credit for.
It won’t work for every condition or every person. But for many dealing with joint pain, tendon trouble, or lingering strains, it offers a hopeful alternative: a chance to heal from within, without surgery, without synthetic drugs, and without months of being sidelined.
If you’ve tried all the usual routes—ice, rest, therapy—and still feel stuck, PRP might just be the body-friendly nudge your system needs to repair itself. And sometimes, that’s exactly what healing should look like.


