
It is still present in more than 120 countries, and the U.S. is seeing an uptick in cases.

By Dr. Robert A. Schwartz
Professor and Head of Dermatology
Rutgers New Jersey Medical School
Rutgers University
Introduction
The word “leprosy” conjures images of biblical plagues, but the disease is still with us today. Caused by infectious bacteria, some 200,000 new cases are reported each year, according to the World Health Organization. In the United States, leprosy has been entrenched for more than a century in parts of the South where people came into contact with armadillos, the principle proven linkage from animal to humans. However, the more recent outbreaks in the Southeast, especially Florida, have not been associated with animal exposure.
What Is Leprosy and Why Is It Resurfacing in the U.S.?
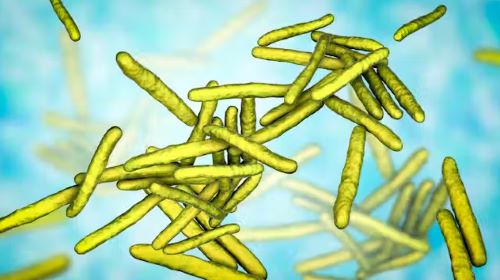
Leprosy is caused by two different but similar bacteria — Mycobacterium leprae and Mycobacterium lepromatosis — the latter having just been identified in 2008. Leprosy, also known as Hansen’s disease, is avoidable. Transmission among the most vulnerable in society, including migrant and impoverished populations, remains a pressing issue.
This age-old neglected tropical disease, which is still present in more than 120 countries, is now a growing challenge in parts of North America.
Leprosy is beginning to occur regularly within parts of the southeastern United States. Most recently, Florida has seen a heightened incidence of leprosy, accounting for many of the newly diagnosed cases in the U.S.
The surge in new cases in central Florida highlights the urgent need for health care providers to report them immediately. Contact tracing is critical to identifying sources and reducing transmission.
Traditional risk factors include zoonotic exposure and having recently lived in leprosy-endemic countries. Brazil, India and Indonesia have each noted more than 10,000 new cases since 2019, according to the World Health Organization data, and more than a dozen countries have reported between 1,000 to 10,000 new cases over the same time period.
Why Was Leprosy Stigmatized Biblical Times?
Evidence suggests that leprosy has plagued civilization since at least the second millennium B.C.
From that time until the mid-20th century, limited treatments were available, so the bacteria could infiltrate the body and cause prominent physical deformities such as disfigured hands and feet. Advanced cases of leprosy cause facial features resembling that of a lion in humans.
Many mutilating and distressing skin disorders such as skin cancers and deep fungal infections were also confused with leprosy by the general public.
Fear of contagion has led to tremendous stigmatization and social exclusion. It was such a serious concern that the Kingdom of Jerusalem had a specialized hospital to care for those suffering from leprosy.
How Infectious Is Leprosy?

Research shows that prolonged in-person contact via respiratory droplets is the primary mode of transmission, rather than through normal, everyday contact such as embracing, shaking hands or sitting near a person with leprosy. People with leprosy generally do not transmit the disease once they begin treatment.
Armadillos represent the only known zoonotic reservoir of leprosy-causing bacteria that threaten humans. These small mammals are common in Central and South America and in parts of Texas, Louisiana, Missouri and other states, where they are sometimes kept as pets or farmed as meat. Eating armadillo meat is not a clear cause of leprosy, but capturing and raising armadillos, along with preparing its meat, are risk factors.
The transmission mechanism between zoonotic reservoirs and susceptible individuals is unknown, but it is strongly suspected that direct contact with an infected armadillo poses a significant risk of developing leprosy. However, many cases reported in the U.S. have demonstrated an absence of either zoonotic exposure or person-to-person transmission outside of North America, suggesting that transmission may be happening where the infected person lives. But in many cases, the source remains an enigma.
Some people’s genetics might make them more susceptible to leprosy infections, or their immune systems are less capable of resisting the disease.
Stigma and discrimination have prevented people from seeking treatment, and as a result, “concealed” cases contribute to transmission.
How Do You Recognize It?
Leprosy primarily affects the skin and peripheral nervous system, causing physical deformity and desensitizing one’s ability to feel pain on affected skin.
It may begin with loss of sensation on whitish patches of skin or reddened skin. As the bacteria spread in the skin, they can cause the skin to thicken with or without nodules. If this occurs on a person’s face, it may rarely produce a smooth, attractive-appearing facial contour known as lepra bonita, or “pretty leprosy.” The disease can progress to causing eyebrow loss, enlarged nerves in the neck, nasal deformities and nerve damage.
The onset of symptoms can sometimes take as long as 20 years because the infectious bacteria have a lengthy incubation period and proliferate slowly in the human body. So presumably many people are infected long before they know that they are.
Fortunately, worldwide efforts to screen for leprosy are being enhanced thanks to organizations like the Order of Saint Lazarus, which was originally founded in the 11th century to combat leprosy, and the Armauer Hansen Research Institute, which conducts immunologic, epidemiological and translational research in Ethiopia. The nongovernmental organization Bombay Leprosy Project in India does the same.
How Treatable Is It?
Leprosy is not only preventable but treatable. Defying stigma and advancing early diagnosis via proactive measures are critical to the mission of controlling and eradicating it worldwide.
Notably, the World Health Organization and other agencies provide multi-drug therapy at no cost to patients.
In addition, vaccine technology to combat leprosy is in the clinical trials stage and could become available in coming years. In studies involving nine-banded armadillos, this protein-based vaccine delayed or diminished leprous nerve damage and kept bacteria at bay. Researchers believe that the vaccine can be produced in a low-cost, highly efficient manner, with the long-term prospect of eradicating leprosy.
If health care professionals, biomedical researchers and lawmakers do not markedly enhance their efforts to eliminate leprosy worldwide, the disease will continue to spread and could become a far more serious problem in areas that have been largely free of leprosy for decades.
The World Health Organization launched a plan in 2021 for achieving zero leprosy.
Originally published by The Conversation, 03.13.2024, under the terms of a Creative Commons Attribution/No derivatives license.


