Pneumonia remains an evolving public health challenge shaped by antimicrobial resistance, emerging pathogens, and global disparities in access to vaccination.

By Matthew A. McIntosh
Public Historian
Brewminate
Introduction
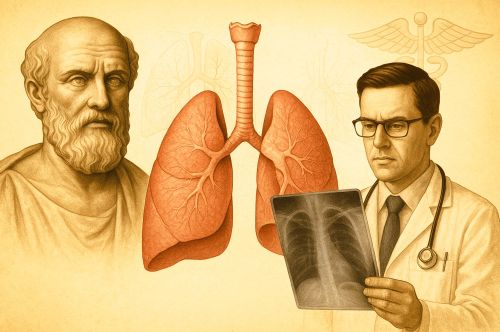
Pneumonia has occupied a central place in the history of medicine for more than two millennia, appearing in some of the earliest surviving clinical writings and continuing to challenge physicians well into the modern era. The disease was described with striking clarity by Hippocrates in the fifth and fourth centuries BCE, whose accounts of fever, chest pain, labored breathing, and sputum established a recognizable clinical pattern that would guide later generations.1
Across the medieval world, scholars working within both Christian and Islamic intellectual traditions preserved and expanded these early observations. Among them, Maimonides provided one of the most refined premodern discussions of respiratory disease, distinguishing forms of pulmonary inflammation with a precision that reflected both deep textual knowledge and extensive bedside experience.2 His descriptions remained influential for centuries and represented one of the high points of medieval clinical reasoning.
Modern understanding of pneumonia emerged only after laboratory science began to transform medicine in the nineteenth century. Researchers such as Edwin Klebs, Carl Friedlander, Albert Frankel, Louis Pasteur, and George Sternberg isolated specific bacteria in inflamed lungs and linked them to cases of acute respiratory illness, setting the foundation for the identification of Streptococcus pneumoniae.3 Their work marked a shift from symptom based interpretation to microbial etiology and placed pneumonia within the rising field of bacteriology.
Despite these advances, pneumonia remained one of the deadliest infectious diseases well into the early twentieth century. It claimed millions of lives each year and commanded particular fear among clinicians. William Osler, whose medical textbook shaped generations of physicians, referred to pneumonia as the Captain of the Men of Death, a phrase that captured the gravity with which the disease was regarded before the advent of effective therapies.4
The discovery of antibiotics in the 1930s and 1940s transformed the prognosis of bacterial pneumonia and dramatically reduced mortality rates across the industrialized world. In the same decades, clinicians identified atypical forms of the disease that behaved differently from classic pneumococcal infections. These atypical pneumonias, including those later attributed to Mycoplasma pneumoniae, signaled a turn toward a more complex understanding of respiratory pathogens.5 By the late twentieth century, rising antibiotic resistance and the development of pneumococcal vaccines drew renewed attention to prevention and public health, ensuring that the long history of pneumonia continued into the era of global medicine.
Pneumonia in Hippocratic Medicine (5th–4th Centuries BCE)

The earliest surviving clinical discussions of pneumonia appear in the Hippocratic corpus, a collection of texts produced on the island of Kos and throughout classical Greece. Hippocratic physicians described acute respiratory illnesses marked by fever, chest pain, productive cough, and labored breathing, features that align with modern clinical presentations of pneumonia. These accounts appear most clearly in Epidemics I and Epidemics III, where the authors recorded bedside observations from real cases and emphasized changes in sputum, patterns of fever, and crisis days.6
Central to Hippocratic interpretation was the humoral framework, which understood disease as an imbalance among bodily fluids. Pneumonia was explained as an inflammation of the chest arising from such imbalance, often accompanied by pleuritic pain that intensified with breathing. Although humoral theory shaped the causal interpretation, the clinical descriptions themselves reflected detailed and systematic observation. Physicians noted that the appearance of sputum, particularly when thick or rust colored, often signaled the progression of the illness and influenced the prognosis.7
Hippocratic writers approached diagnosis as a matter of pattern recognition. They advised practitioners to pay attention to respiratory difficulty, changes in voice, the presence of chills, and the timing of expectoration. The emphasis on crisis days, points at which a disease would turn toward recovery or decline, also informed their understanding of pneumonia. These crisis periods were mapped onto larger theories of disease cycles and provided a predictive framework for the course of acute illnesses.8
The limitations of Hippocratic knowledge stemmed from the absence of anatomical and pathological investigation. Without dissection or a concept of infectious agents, Hippocratic medicine could not identify the underlying mechanisms of pulmonary inflammation. Yet the accuracy of the clinical features they recorded meant that later physicians across different cultures recognized the continuity of these symptoms. Their work became one of the foundational sources for respiratory disease understanding throughout antiquity and the medieval world.9
Roman, Late Antique, and Early Medieval Interpretations

Roman and late antique physicians inherited the clinical descriptions found in the Hippocratic corpus and incorporated them into more elaborate theoretical systems. Among these figures, Galen proved especially influential. His commentaries linked pulmonary inflammation to disruptions of the humors and described how environmental factors, temperament, and diet shaped susceptibility to respiratory disease. Although framed within a philosophical structure, Galen’s remarks preserved the practical details of Hippocratic symptomatology, including fever, cough, and pain localized to the chest.10
Galen’s influence continued throughout late antiquity as medical handbooks circulated across the Mediterranean. Authors such as Oribasius and Aëtius of Amida summarized Galenic teaching on chest diseases and offered therapeutic recommendations grounded in both humoral theory and empirical observation. They relied heavily on Hippocratic case patterns, reinforcing the continuity of symptom based diagnosis. These compendia introduced incremental refinements but did not depart from the core understanding of pneumonia as a form of internal inflammation associated with disordered bodily fluids.11
As the political and cultural landscape of the Mediterranean changed, medical traditions migrated and adapted. Greek and Syriac scholars preserved clinical writings and translated major treatises, including those by Galen, into new linguistic contexts. These translations allowed respiratory disease concepts to reach physicians who worked outside the classical world and laid the foundation for their incorporation into emerging Islamic medical scholarship. The emphasis on careful observation remained central to the diagnostic process across these traditions.12
Early medieval medical writers in the Latin West continued to rely on abbreviated Galenic summaries. While their texts often lacked the depth found in late antique collections, they maintained the core symptoms associated with pulmonary inflammation and recognized the severity of conditions involving pleuritic pain and productive cough. Their therapeutic approaches, shaped by monastic scriptoria and local resources, reflected continuity rather than innovation. Although anatomical knowledge remained limited, the clinical vocabulary of pneumonia proved stable enough to survive the fragmentation of late Roman intellectual life.13
By the time Islamic scholars began to systematize and expand classical medicine, the symptom based framework inherited from Hippocrates and Galen was firmly established. This tradition would eventually support the far more detailed analyses produced by scholars such as Maimonides, whose work represented a new level of clinical clarity while remaining rooted in the ancient descriptions of pulmonary disease.14
Maimonides and Medieval Islamic Clinical Precision (12th Century)

Medical scholarship in the medieval Islamic world preserved and expanded the classical tradition, but few physicians matched the clarity and systematic rigor of Maimonides. Working in twelfth century Egypt, he drew on Greek, Syriac, and earlier Arabic authorities, yet relied heavily on his own observations at the bedside. His clinical writings reveal a careful attention to symptoms that distinguished respiratory illnesses with a precision not found in most earlier treatises. In his Medical Aphorisms, he addressed disorders of the lungs with a focus on fever, the character of the cough, and the quality of sputum, all of which he treated as essential in differentiating forms of pulmonary disease.15
Maimonides also produced individual treatises that offered more sustained analysis of respiratory conditions. His Treatise on Asthma contained extended reflections on breathing difficulty, chest constriction, and the role of environmental factors in the onset of illness. Although the work did not directly isolate pneumonia as a separate disease category in the modern sense, he described patterns of pleuritic pain and fever that strongly align with pneumonic inflammation. His attention to triggers, climatic conditions, and physical exertion reflected a broader commitment to understanding disease within both physiological and environmental contexts.16
A notable feature of Maimonides’ approach was his effort to integrate textual learning with empirical practice. He frequently compared inherited descriptions from Galen and Hippocratic writers with the symptoms he encountered in daily medical work. Where the ancient authorities offered divergent explanations, he emphasized clinical observation as the final measure. This method allowed him to distinguish between superficial similarities in respiratory symptoms and the deeper patterns that separated pneumonia, pleurisy, asthma, and other chest conditions.17
Despite these advances, Maimonides operated within the humoral theory that shaped all premodern medicine. He attributed pulmonary inflammation to imbalances in bodily fluids and interpreted fever as a sign of the body’s attempt to resolve these disturbances. Even so, the precision of his symptom based descriptions marked a significant development in the long history of respiratory disease. His work served as a vital bridge between classical medical theory and later traditions, ensuring that the careful observational framework surrounding pneumonia remained intact as medicine moved toward the anatomical and pathological sciences of the early modern world.18
Pneumonia in Early Modern and Enlightenment Medicine

The revival of anatomical study during the Renaissance marked a significant shift in how physicians approached diseases of the chest. Increasing acceptance of human dissection allowed scholars to correlate symptoms observed during life with structural changes discovered after death. Although the humoral framework remained dominant, anatomical pathology provided new tools for understanding pulmonary inflammation. Early anatomists described regions of lung tissue that appeared firm, heavy, or discolored, and these findings helped refine the distinction between different forms of respiratory disease.19
By the seventeenth century, physicians such as Thomas Sydenham promoted more systematic clinical description and insisted that diseases should be classified based on observable patterns. Sydenham treated epidemics and acute respiratory disorders with an approach grounded in bedside observation rather than philosophical speculation. While he did not identify pneumonia as a unique microbial illness, his commitment to describing diseases as they appeared in nature contributed to a broader methodological shift that emphasized careful clinical recognition.20
The eighteenth century witnessed further development through the rise of pathological anatomy in Europe. Giovanni Battista Morgagni’s extensive case studies linked symptoms recorded during life with autopsy findings and provided some of the earliest sustained correlations between chest pain, fever, and areas of pulmonary consolidation. Morgagni described solidified lung tissue in patients who had suffered from acute respiratory illness, a finding that corresponded closely with later definitions of lobar pneumonia. His work represented a decisive step away from theoretical speculation and toward the anatomical basis of disease.21
Despite these advances, the cause of pneumonia remained unknown. Physicians could identify diseased tissue, describe the spread of inflammation, and differentiate between lobar and bronchial patterns, yet no explanation existed for why the condition arose or why it behaved with such severity. Treatments remained largely supportive and often ineffective. This period, however, laid the intellectual groundwork for the bacteriological discoveries of the nineteenth century by demonstrating that disease had specific local manifestations that could be studied systematically.22
The Birth of Bacteriology and Identification of Pneumococcus (Late 19th Century)

The late nineteenth century transformed the understanding of pneumonia through the rise of bacteriology, a field that allowed scientists to identify microorganisms as causes of specific diseases. Prior to this period, pneumonia had been classified largely by symptoms and anatomical findings, but the underlying mechanism remained obscure. Microscopy, culture techniques, and improved staining methods made it possible to isolate pathogens directly from diseased tissue. These tools provided the foundation for a new model of respiratory illness, one that linked clinical presentation to identifiable microbial agents.23
Edwin Klebs was one of the earliest researchers to identify bacteria in the lungs of patients who had died from acute infections. His work did not definitively isolate the pneumococcus, but it helped establish the principle that infectious diseases could be studied through the organisms they produced. Klebs’ investigations encouraged other scientists to search for specific bacterial agents responsible for recognizable disease patterns.24
Carl Friedlander advanced this work by describing a capsulated bacillus in patients with pneumonia, an organism later classified as Klebsiella pneumoniae. Although Friedlander believed this bacterium to be the principal cause of pneumonia, subsequent research showed that it represented only one form of the disease. His findings nevertheless demonstrated the importance of careful staining techniques and contributed to the broader effort to classify bacterial pathogens by morphology and behavior.25
Albert Frankel and Louis Pasteur independently identified a different organism associated with pneumonia, a lancet shaped diplococcus that appeared consistently in cases of acute lobar inflammation. Pasteur’s research in France and Frankel’s work in Germany established that this organism could cause disease in animals and could be recovered reliably from infected lung tissue. Their findings provided strong evidence that pneumonia often resulted from a specific bacterial pathogen rather than a generalized inflammatory process.26
George Sternberg, working in the United States, conducted parallel investigations and successfully isolated the same diplococcus. His experiments confirmed that the organism, later named Streptococcus pneumoniae, was capable of producing experimental pneumonia in animals and could be transmitted from one host to another. Sternberg’s research helped solidify the recognition of pneumococcus as a major etiologic agent and placed pneumonia firmly within the framework of infectious disease.27
Pneumonia as the “Captain of the Men of Death” and the Mortality Crisis
By the early twentieth century, pneumonia had become one of the leading causes of death in Europe and the United States. Hospital records from the late nineteenth and early twentieth centuries consistently showed high mortality among adults who developed acute lobar pneumonia, especially older patients. Physicians observed that the disease often progressed rapidly and resisted the therapeutic approaches available at the time. Despite the improved diagnostic precision offered by bacteriology and pathological anatomy, clinical outcomes remained grim.28
William Osler captured the prevailing medical anxiety in his Principles and Practice of Medicine, where he described pneumonia as the Captain of the Men of Death. His remark reflected both the frequency with which the disease claimed lives and the sense of inevitability that surrounded severe cases before the introduction of effective treatments. Osler emphasized that age played a significant role in prognosis, noting that elderly patients often lacked the physiological reserves needed to survive acute respiratory infections.29
Public health records from the early twentieth century reinforce Osler’s evaluation. Before antibiotics, pneumonia consistently ranked among the top causes of mortality in the United States. Studies of urban hospital populations revealed mortality rates that frequently exceeded twenty percent in adults and rose even higher among the elderly. These figures remained stable year after year, which underscored the limited impact of available therapies and the difficulty physicians faced in altering the course of the disease.30
Scientific literature of the period identified pneumococcus as a major contributor to these high death rates, but the recognition of the organism did not immediately lead to successful treatment. Serum therapies provided some benefit but were inconsistent and depended heavily on the specific pneumococcal type involved. As a result, clinicians continued to rely on supportive care, careful monitoring, and the hope that patients would reach a natural crisis point that favored recovery. The absence of reliable antimicrobial therapy made pneumonia a condition that physicians feared and patients rarely survived once severe symptoms appeared.31
The persistence of high mortality during this period demonstrates the profound impact pneumonia had on global health before the advent of modern medicine. It remained a defining cause of death in the industrial world and a central focus of clinical education. The crisis created by pneumonia’s lethality would ultimately drive scientific efforts that culminated in new treatments during the 1930s and 1940s, transforming what had long been one of the most feared diseases into a condition that could often be managed successfully.32
Therapeutic Turning Point: The 1930s and the Rise of Antibiotics

The introduction of new therapies in the 1930s marked a decisive shift in the management of pneumonia. Before this period, treatment relied primarily on supportive care, cautious monitoring, and the limited use of type specific pneumococcal antiserum. While antiserum therapy brought measurable reductions in mortality for certain pneumococcal types, it required rapid diagnosis, specialized production methods, and significant clinical expertise. Mortality among adults, especially those with type III pneumococcus, remained high even under optimal conditions.33
Sulfonamide drugs brought the first transformative change. Prontosil, introduced in the mid-1930s, demonstrated clear reductions in pneumonia mortality across multiple clinical studies. Its ability to inhibit bacterial growth made it dramatically more effective than previous therapies, and hospitals that adopted sulfonamides reported steep declines in deaths from pneumococcal pneumonia. The drug’s broad availability and ease of administration allowed physicians to treat patients earlier in the course of illness, and its impact served as a precursor to the even greater changes that would follow.34
Penicillin, introduced in the early 1940s, completed this therapeutic revolution. Clinical trials during the Second World War confirmed its ability to treat pneumococcal infections with a level of reliability that surpassed all previous treatments. Penicillin rapidly reduced bacterial load, shortened the duration of fever, and prevented many of the complications that had previously contributed to high mortality. As production expanded, the drug became widely accessible and reshaped expectations for the management of pneumonia across both military and civilian hospitals.35
The combined effects of sulfonamides and penicillin produced a dramatic global decline in pneumonia mortality by the mid twentieth century. Public health statistics from the 1930s to the 1950s show a steep downward trajectory in deaths from respiratory infections, a shift directly tied to the availability of effective antimicrobial therapy. These developments altered the clinical landscape and changed pneumonia from a disease long associated with inevitability and death into one that could be managed successfully in most cases. The therapeutic transformation of this period stands as one of the most significant milestones in the history of infectious disease.36
Discovery of Atypical Pneumonia and Viral Agents (1930s–1960s)
During the 1930s, clinicians began to recognize that not all pneumonias behaved like classic pneumococcal infections. Patients appeared with prolonged fever, nonproductive cough, and diffuse radiographic findings that did not match the lobar patterns associated with pneumococcus. These cases tended to progress more slowly, often occurred in younger individuals, and frequently produced milder clinical courses. Physicians described them as primary atypical pneumonia, a term that signaled both diagnostic uncertainty and the growing realization that respiratory disease encompassed more than a single bacterial entity.37
Epidemiological studies during this decade provided early clues that atypical pneumonia differed fundamentally from traditional forms. Outbreaks occurred in patterns unlike pneumococcal epidemics and appeared to spread more readily among close contacts, particularly in military barracks and school environments. Laboratory tests often failed to isolate pneumococcus from these patients, reinforcing the idea that another agent was responsible. As researchers documented these episodes, they developed a clearer sense that pneumonia could arise from diverse causes that required new investigative approaches.38
The search for the agent responsible for these atypical cases intensified during the early 1940s. A research group led by Monroe Eaton identified an infectious filtrable agent capable of producing pneumonia in experimental animals. Because the agent passed through filters that trapped known bacteria, scientists initially believed it to be viral. This conclusion reflected the tools available at the time, as standard bacteriological methods were unable to detect organisms that lacked a rigid cell wall or grew slowly under laboratory conditions. The Eaton agent became a focal point for ongoing research into nonpneumococcal respiratory infections.39
Throughout the postwar period, investigators attempted to determine the biological nature of the Eaton agent and to reproduce the disease in controlled settings. These efforts revealed that the organism behaved differently from traditional bacteria and exhibited growth characteristics that resembled neither viruses nor typical microbial pathogens. The difficulty of cultivating the agent hindered early attempts at definitive identification, but the persistence of clinical outbreaks kept the problem before the scientific community. Case reports and experimental work gradually narrowed the range of possibilities regarding the organism’s classification.40
The decisive breakthrough came in the 1960s, when the Eaton agent was successfully grown in tissue culture and identified as Mycoplasma pneumoniae. This organism belonged to a group of wall-less bacteria capable of passing through standard bacteriological filters, which explained its earlier misclassification as viral. Its identification provided a clear explanation for the large number of atypical pneumonia cases that had defied traditional diagnostic methods during the previous decades. The recognition of Mycoplasma pneumoniae as a human pathogen expanded the taxonomy of respiratory infections and reshaped the diagnostic landscape.41
The discovery of atypical pneumonia contributed to a broader reevaluation of respiratory disease by demonstrating that clinical presentations could not reliably indicate the underlying etiology. It emphasized the need for new laboratory techniques, improved culture methods, and more refined diagnostic tools. As physicians incorporated this knowledge into clinical practice, pneumonia increasingly came to be understood as a heterogeneous group of conditions rather than a single disease entity. This conceptual shift prepared the ground for later advances in virology, immunology, and antimicrobial therapy, all of which would further refine the understanding of respiratory illness.42
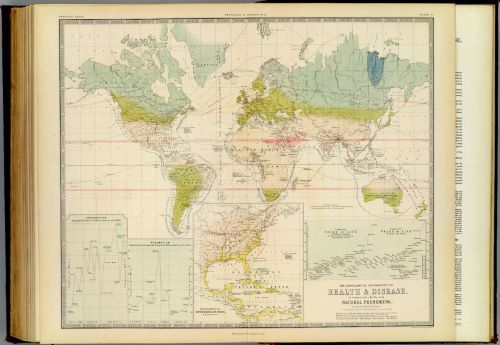
Antibiotic Resistance, Public Health, and Vaccination (1990s–Present)
By the late twentieth century, the widespread use of antibiotics transformed the clinical management of pneumonia, but it also created new challenges as resistant strains of Streptococcus pneumoniae began to emerge. Researchers documented rising rates of resistance to penicillin and multiple other antimicrobial agents, particularly in regions with heavy antibiotic use. These findings raised concerns that the remarkable therapeutic gains made during the mid century could erode without coordinated public health responses. Laboratory surveillance programs expanded during the 1990s, providing clearer data on resistance trends and guiding early policy recommendations.43
Antibiotic resistance also changed how clinicians approached the selection of empirical therapy for community acquired pneumonia. Guidelines issued by professional societies incorporated local resistance data and emphasized the importance of covering both typical and atypical pathogens. Physicians increasingly relied on combination therapy or broader spectrum drugs in areas with high rates of resistant pneumococcal isolates. These adjustments reflected the growing complexity of managing bacterial respiratory infections in an era when older, reliable treatments no longer guaranteed consistent success.44
The development of pneumococcal conjugate vaccines represented one of the most effective strategies for countering the rise of resistant strains. The heptavalent pneumococcal conjugate vaccine, introduced in 2000, reduced invasive pneumococcal disease in children and indirectly lowered rates among adults through herd immunity. Later vaccines with expanded serotype coverage, including the thirteen valent formulation, further decreased infections caused by the most clinically significant strains. These reductions not only improved overall disease control but also helped limit the spread of resistant serotypes within communities.45
Public health initiatives throughout the early twenty first century emphasized vaccination as a critical tool in preventing pneumonia among vulnerable populations. Recommendations targeted young children, older adults, and individuals with chronic medical conditions who faced higher risks of severe disease. International guidelines also promoted vaccination in low and middle income countries, where pneumonia remained a leading cause of childhood mortality. The global focus on immunization underscored a broader shift in pneumonia prevention, extending beyond treatment and toward reducing disease incidence itself.46
The persistence of antibiotic resistance and the emergence of new respiratory pathogens ensured that pneumonia remained a significant public health concern. Recent strategies have integrated vaccination programs, antimicrobial stewardship, and improved diagnostic testing to manage both bacterial and atypical forms of the disease. These efforts reflect the culmination of centuries of medical advancement, linking ancient clinical observation with modern microbiology and epidemiology. Pneumonia’s long history continues into the present as clinicians, researchers, and public health officials work to protect populations from a disease that has shaped medical practice from antiquity to the contemporary world.47
Conclusion
The long history of pneumonia reveals the continuity of clinical observation across cultures and centuries. Hippocrates established the first recognizable descriptions of the disease, and these accounts influenced physicians throughout the Greco Roman world. Medieval Islamic scholars, particularly Maimonides, advanced this tradition by integrating inherited texts with direct bedside practice, preserving a clinical framework that allowed respiratory diseases to be described in increasingly precise terms. Their work ensured that medicine entered the early modern period with a stable vocabulary for interpreting pulmonary illness.48
The rise of anatomical pathology during the Renaissance and Enlightenment reshaped this inherited knowledge by linking symptoms to structural changes in the lung. Although the causes of pneumonia remained unknown, physicians gained a deeper understanding of the patterns of disease and the importance of localized lesions. This anatomical perspective prepared the ground for the breakthroughs of the nineteenth century, when bacteriologists identified specific microbial agents responsible for acute pulmonary infections. Their success transformed pneumonia from a condition interpreted through humoral theory into a disease understood within the growing science of infectious pathology.49
Even with these advances, pneumonia remained a major cause of death until the therapeutic revolution of the 1930s and 1940s. The introduction of sulfonamides and penicillin dramatically reduced mortality rates and changed clinical expectations regarding the course of the disease. These therapies, combined with improved diagnostic methods, allowed physicians to treat bacterial pneumonia with unprecedented confidence. Later research revealed that pneumonia was not a single disease but a family of respiratory conditions that included atypical and viral forms. The identification of Mycoplasma pneumoniae highlighted the need for expanded laboratory approaches capable of detecting organisms that did not conform to traditional bacteriological methods.50
Pneumonia remains an evolving public health challenge shaped by antimicrobial resistance, emerging pathogens, and global disparities in access to vaccination. Efforts to control the disease now depend on integrating scientific knowledge with coordinated preventive strategies. The trajectory from ancient bedside observation to modern epidemiology demonstrates how medicine adapts to new tools, new theories, and new threats. Across this long history, pneumonia has served as a measure of medical understanding itself, reflecting the strengths and limitations of each era while continually prompting further inquiry into the nature of respiratory illness.51
Appendix
Footnotes
- Hippocrates, Hippocratic Writings, ed. G. E. R. Lloyd (London: Penguin Classics, 1983), selections from Epidemics and Aphorisms.
- Maimonides, Medical Aphorisms of Moses Maimonides, trans. Fred Rosner (Philadelphia: Jewish Publication Society, 1970).
- Thomas D. Brock, Milestones in Microbiology (Washington, D.C.: ASM Press, 1961).
- William Osler, The Principles and Practice of Medicine (New York: D. Appleton, 1892).
- F. W. Eaton et al., “Primary Atypical Pneumonia,” Journal of Experimental Medicine 82, no. 2 (1945).
- Hippocrates, Hippocratic Writings, 148–165.
- Ibid., 150–158; Vivian Nutton, Ancient Medicine (London: Routledge, 2004), 58–63.
- Hippocrates, Aphorisms, in Hippocratic Writings, 208–215.
- Nutton, Ancient Medicine, 61–66.
- Galen, On the Affected Parts, trans. Rudolph E. Siegel (Basel: Karger, 1976), 113–118.
- Oribasius, Medical Collections, trans. John Scarborough (Leiden: Brill, 1997), 45–52; Aëtius of Amida, The Medical Books of Aëtius of Amida, ed. Alexander Olivieri (Leipzig: Teubner, 1935).
- Sebastian Brock, “Greek into Syriac: The Transmission of Greek Medical Texts into Syriac,” Aram 3 (1991): 139–151.
- Faith Wallis, Medieval Medicine: A Reader (Toronto: University of Toronto Press, 2010), 56–63.
- Peter E. Pormann and Emilie Savage Smith, Medieval Islamic Medicine (Edinburgh: Edinburgh University Press, 2007), 98–104.
- Maimonides, Medical Aphorisms of Moses Maimonides, 65–78.
- Maimonides, Treatise on Asthma, trans. Gerrit Bos (Provo: Brigham Young University Press, 2002), 15–34.
- Bos, introduction to Treatise on Asthma, 1–12.
- Pormann and Savage Smith, Medieval Islamic Medicine, 98–104.
- Katharine Park, Secrets of Women: Gender, Generation, and the Origins of Human Dissection (New York: Zone Books, 2006), 173–182.
- Thomas Sydenham, The Works of Thomas Sydenham, trans. John Pechey (London: R. Wellington, 1696), 112–120.
- Giovanni Battista Morgagni, The Seats and Causes of Diseases Investigated by Anatomy, trans. Benjamin Alexander (London: A. Millar, 1769), vol. 1, 258–271.
- Andrew Cunningham, The Anatomical Renaissance (Aldershot: Scolar Press, 1997), 233–240.
- Erwin H. Ackerknecht, A Short History of Medicine (Baltimore: Johns Hopkins University Press, 1955), 156–165.
- Thomas D. Brock, Milestones in Microbiology, 67–69.
- Carl Friedlander, “Ueber die Schizomyceten bei der acuten Lungenentzündung,” Virchows Archiv 87 (1882): 319–324.
- Albert Frankel, “Ueber die Aetiologie der Pneumonie,” Deutsche Medizinische Wochenschrift 10 (1884): 969–972; Louis Pasteur, “Note sur la maladie nouvelle provoquée par le microbe pneumonique,” Comptes Rendus de l’Académie des Sciences 92 (1881): 264–267.
- George M. Sternberg, “A New Pathogenic Organism in the Saliva,” The Bulletin of the National Board of Health 4 (1881): 74–76.
- George Rosen, A History of Public Health (Baltimore: Johns Hopkins University Press, 1943), 254–260.
- William Osler, The Principles and Practice of Medicine, 108–110.
- D. A. Morens, J. K. Taubenberger, and A. S. Fauci, “Pneumonia before Antibiotics: The History of the Pneumococcus and Its Role in Mortality,” Journal of Infectious Diseases 169, no. 1 (1994): 16–23.
- Rosen, A History of Public Health, 257–259.
- Morens, Taubenberger, and Fauci, “Pneumonia before Antibiotics,” 21–23.
- Morens, Taubenberger, and Fauci, “Pneumonia before Antibiotics,” 19–21.
- John Parascandola, The Development of American Pharmacology (Baltimore: Johns Hopkins University Press, 1992), 142–148.
- Gladys L. Hobby, Penicillin: Meeting the Challenge (New Haven: Yale University Press, 1985), 55–67.
- Rosen, A History of Public Health (Baltimore: Johns Hopkins University Press, 1993), 295–302.
- Thomas M. File Jr., “Community Acquired Pneumonia,” Lancet 362, no. 9400 (2003): 1991–2001.
- John F. Murray and Graham L. Williams, Respiratory Medicine (Philadelphia: W. B. Saunders, 1988), 212–215.
- Monroe D. Eaton, G. Meiklejohn, and C. van Herick, “Studies on the Etiology of Primary Atypical Pneumonia,” Journal of Experimental Medicine 82, no. 4 (1945): 317–328.
- Frederick L. Dunn and Thomas D. Y. Chan, “Atypical Pneumonias and Their Etiology,” British Medical Journal 2 (1954): 1214–1217.
- Leonard Hayflick, “The Mycoplasma Story,” Journal of Infectious Diseases 134, no. 4 (1976): 316–323.
- Murray and Williams, Respiratory Medicine, 215–219.
- Centers for Disease Control and Prevention, “Defining the Problem of Drug Resistant Pneumococcus,” Morbidity and Mortality Weekly Report 45, no. 1 (1996): 1–14.
- Lionel A. Mandell et al., “Infectious Diseases Society of America and American Thoracic Society Consensus Guidelines on the Management of Community Acquired Pneumonia,” Clinical Infectious Diseases 44, suppl. 2 (2007): S27–S72.
- Cynthia G. Whitney et al., “Decline in Invasive Pneumococcal Disease after the Introduction of Protein Conjugate Vaccine,” New England Journal of Medicine 348, no. 18 (2003): 1737–1746.
- World Health Organization, Pneumococcal Vaccines WHO Position Paper (Geneva: WHO Press, 2012), 129–144.
- Keith P. Klugman, Thomas M. File Jr., and Cynthia G. Whitney, “Pneumococcal Disease and Prevention in the Twenty First Century,” Lancet 378, no. 9807 (2011): 439–452.
- Nutton, Ancient Medicine, 58–66.
- Ackerknecht, A Short History of Medicine, 149–170.
- D. A. Morens, J. K. Taubenberger, and A. S. Fauci, “Pneumonia before Antibiotics,” 19–23.
- Klugman, File, and Whitney, “Pneumococcal Disease and Prevention,” 439–452.
Bibliography
- Ackerknecht, Erwin H. A Short History of Medicine. Baltimore: Johns Hopkins University Press, 1955.
- Aëtius of Amida. The Medical Books of Aëtius of Amida. Edited by Alexander Olivieri. Leipzig: Teubner, 1935.
- Brock, Thomas D. Milestones in Microbiology. Washington, D.C.: ASM Press, 1961.
- Brock, Sebastian. “Greek into Syriac: The Transmission of Greek Medical Texts into Syriac.” Aram 3 (1991): 139–151.
- Centers for Disease Control and Prevention. “Defining the Problem of Drug Resistant Pneumococcus.” Morbidity and Mortality Weekly Report 45, no. 1 (1996): 1–14.
- Cunningham, Andrew. The Anatomical Renaissance. Aldershot: Scolar Press, 1997.
- Dunn, Frederick L., and Thomas D. Y. Chan. “Atypical Pneumonias and Their Etiology.” British Medical Journal 2 (1954): 1214–1217.
- Eaton, Monroe D., G. Meiklejohn, and C. van Herick. “Studies on the Etiology of Primary Atypical Pneumonia.” Journal of Experimental Medicine 82, no. 4 (1945): 317–328.
- File, Thomas M. Jr. “Community Acquired Pneumonia.” Lancet 362, no. 9400 (2003): 1991–2001.
- Frankel, Albert. “Ueber die Aetiologie der Pneumonie.” Deutsche Medizinische Wochenschrift 10 (1884): 969–972.
- Friedlander, Carl. “Ueber die Schizomyceten bei der acuten Lungenentzündung.” Virchows Archiv 87 (1882): 319–324.
- Hayflick, Leonard. “The Mycoplasma Story.” Journal of Infectious Diseases 134, no. 4 (1976): 316–323.
- Hippocrates. Hippocratic Writings. Edited by G. E. R. Lloyd. London: Penguin Classics, 1983.
- Hobby, Gladys L. Penicillin: Meeting the Challenge. New Haven: Yale University Press, 1985.
- Klugman, Keith P., Thomas M. File Jr., and Cynthia G. Whitney. “Pneumococcal Disease and Prevention in the Twenty First Century.” Lancet 378, no. 9807 (2011): 439–452.
- Mandell, Lionel A., et al. “Infectious Diseases Society of America and American Thoracic Society Consensus Guidelines on the Management of Community Acquired Pneumonia.” Clinical Infectious Diseases 44, suppl. 2 (2007): S27–S72.
- Maimonides. Medical Aphorisms of Moses Maimonides. Translated by Fred Rosner. Philadelphia: Jewish Publication Society, 1970.
- ———. Treatise on Asthma. Translated by Gerrit Bos. Provo: Brigham Young University Press, 2002.
- Morgagni, Giovanni Battista. The Seats and Causes of Diseases Investigated by Anatomy. Translated by Benjamin Alexander. London: A. Millar, 1769.
- Morens, D. A., J. K. Taubenberger, and A. S. Fauci. “Pneumonia before Antibiotics: The History of the Pneumococcus and Its Role in Mortality.” Journal of Infectious Diseases 169, no. 1 (1994): 16–23.
- Murray, John F., and Graham L. Williams. Respiratory Medicine. Philadelphia: W. B. Saunders, 1988.
- Nutton, Vivian. Ancient Medicine. London: Routledge, 2004.
- Oribasius. Medical Collections. Translated by John Scarborough. Leiden: Brill, 1997.
- Osler, William. The Principles and Practice of Medicine. New York: D. Appleton, 1892.
- Park, Katharine. Secrets of Women: Gender, Generation, and the Origins of Human Dissection. New York: Zone Books, 2006.
- Parascandola, John. The Development of American Pharmacology. Baltimore: Johns Hopkins University Press, 1992.
- Pasteur, Louis. “Note sur la maladie nouvelle provoquée par le microbe pneumonique.” Comptes Rendus de l’Académie des Sciences 92 (1881): 264–267.
- Pormann, Peter E., and Emilie Savage Smith. Medieval Islamic Medicine. Edinburgh: Edinburgh University Press, 2007.
- Rosen, George. A History of Public Health. Baltimore: Johns Hopkins University Press, 1943.
- Scarborough, John. Medical Collections of Oribasius. Leiden: Brill, 1997.
- Sternberg, George M. “A New Pathogenic Organism in the Saliva.” The Bulletin of the National Board of Health 4 (1881): 74–76.
- Sydenham, Thomas. The Works of Thomas Sydenham. Translated by John Pechey. London: R. Wellington, 1696.
- Whitney, Cynthia G., et al. “Decline in Invasive Pneumococcal Disease after the Introduction of Protein Conjugate Vaccine.” New England Journal of Medicine 348, no. 18 (2003): 1737–1746.
- World Health Organization. Pneumococcal Vaccines WHO Position Paper. Geneva: WHO Press, 2012.
- Wallis, Faith. Medieval Medicine: A Reader. Toronto: University of Toronto Press, 2010.
Originally published by Brewminate, 11.17.2025, under the terms of a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International license.