

Peptide stacking has emerged as one of the most visible examples of the widening divide between scientific evidence and wellness culture.

By Matthew A. McIntosh
Public Historian
Brewminate
Introduction
A new wellness trend called “peptide stacking” has surged across social media, boutique clinics, and influencer circles, promising anti-aging benefits, rapid muscle recovery, and accelerated fat loss. The practice involves injecting combinations of unapproved peptides, many of which are legally sold online as “research chemicals” despite the fact that they are being marketed for human use. These compounds lack meaningful human trial data, carry unclear long-term risks, and are already tied to a rapidly expanding gray market.
This trend has intensified as high-profile figures amplify it. Robert F. Kennedy Jr., who has promoted peptides through his “Make America Healthy Again” movement, argues that federal regulators should loosen restrictions despite the absence of robust clinical evidence. Meanwhile, medical experts warn that the products are not approved drugs, are often misbranded, and can expose users to contamination, dosing inconsistencies, and harmful interactions.
The regulatory tension surrounding peptides stands in sharp contrast to the administration’s approach to proven medicines. While President Trump recently negotiated a plan to lower costs for GLP-1 weight loss drugs, his political allies continue attacking long-established scientific consensus on vaccines and even common household medications. This contradictory stance has created fertile ground for alternative treatments to flourish without the safeguards normally required for therapies injected directly into the human body.
As the craze accelerates, scientists stress that peptide stacking remains an uncontrolled human experiment. Without rigorous clinical trials, transparent manufacturing standards, or regulatory oversight, consumers are left navigating a marketplace where hype and hope outpace evidence. The question now is whether the rush toward these untested therapies reflects genuine innovation or yet another iteration of the wellness industry’s recurring cycle of high-risk snake oil dressed as modern science.
What Is Peptide Stacking?

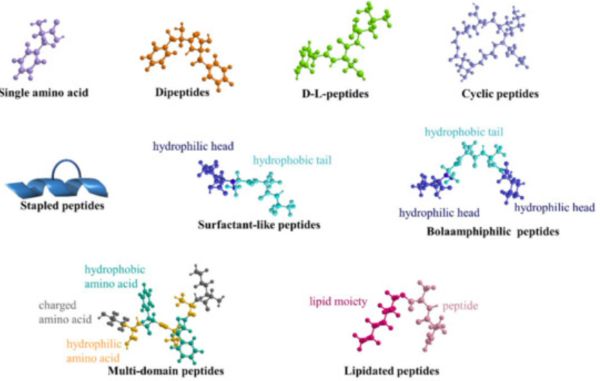
Peptides are short chains of amino acids that act as signaling molecules in the body, regulating everything from tissue repair to hormone activity. Some peptides, such as insulin, are approved prescription drugs with decades of clinical evidence behind them. But the substances fueling the current craze belong to a different category. They are experimental compounds with little to no human testing, many of which are synthesized in overseas labs and sold online under disclaimers like “for research use only.”
“Peptide stacking” refers to combining two or more of these unapproved compounds in an effort to multiply their effects. Stacks often include substances such as BPC-157, TB-500, and blends of CJC-1295 with ipamorelin, all marketed for anti-aging, muscle recovery, weight loss, or cosmetic enhancement. The problem, according to experts, is that many of these peptides have only been tested in animals or in limited early-stage research. There is no established safe dosage, no understanding of long-term effects, and no evidence showing how multiple peptides interact once injected together.
Despite these gaps, stacking has become appealing because it mimics the customization of hormone therapy or pharmaceutical regimens while sidestepping the regulatory pathway that ensures safety. For wellness enthusiasts, it is presented as a kind of advanced biohacking. For clinicians and researchers, it raises the alarm that consumers are experimenting on themselves with compounds that function as drugs but lack the most basic protections of pharmaceutical oversight.
The Rise of the Trend and the Gray Market
The peptide-stacking boom has accelerated through a mix of influencer marketing, celebrity endorsements, and wellness-clinic promotions. The trend has spread rapidly across TikTok, Instagram, and podcast networks where self-styled biohackers frame injectable peptides as a shortcut to youth, vitality, and peak performance. Videos demonstrating how to self-inject compounds labeled “not for human use” have garnered millions of views, helping normalize an activity that occupies a legal gray zone.
A parallel growth channel has emerged in boutique wellness clinics that offer peptide injections as premium anti-aging or fitness services. NBC’s health reporting notes that clinics across the country have begun advertising peptide blends alongside IV drips and hormone therapy, even though the substances lack approval from the Food and Drug Administration. Clinicians acknowledged that demand has spiked dramatically, driven by patients who believe peptides are safer or more “natural” than pharmaceuticals despite the absence of clinical evidence.
Online sellers play a significant role in sustaining the market. Many operate through websites that openly sell peptides in vials while shielding themselves with disclaimers such as “for laboratory research only.” This labeling tactic allows vendors to avoid drug-safety obligations even when consumers are clearly purchasing the products to inject them. Some of these peptides are manufactured in unregulated facilities, raising concerns about sterility, contamination, and potency.
The rising interest in peptide stacks also mirrors the broader cultural momentum created by GLP-1 weight-loss drugs such as Ozempic and Wegovy. Peptides have become synonymous with cutting-edge body modification, even when the compounds being used have no clinical testing behind them. The success of legitimate GLP-1 medications has created an appetite for any substance branded as a “peptide,” allowing experimental blends to flow into the market under the guise of innovative health technology.
Regulatory Status and Safety Concerns

Under federal law, any injectable substance marketed to produce a health benefit is considered a drug, which means it must undergo clinical trials and receive approval from the Food and Drug Administration. The FDA has repeatedly stated that most peptides currently being sold online or through wellness clinics have not met those standards. In its official guidance on bulk drug substances, the agency classifies many popular peptides in a category reserved for compounds that pose significant safety concerns or lack sufficient evidence to justify clinical use. This includes substances frequently featured in peptide stacks such as BPC-157 and TB-500.
Investigations show that companies often bypass regulation by labeling peptides as “research chemicals” even as they are promoted by influencers for direct human injection. The AP found that several products were produced in facilities with little oversight and were sold with no guarantees of sterility, purity, or accurate dosing. Medical experts have warned that contaminants or incorrect concentrations in these vials could result in infections, allergic reactions, or metabolic complications.
Safety concerns extend beyond quality control. A number of these peptides have been tested only in animals, and many have never undergone controlled human trials. Scientists have stressed that the long-term effects remain unknown, especially when consumers combine multiple peptides with overlapping biological pathways. Some peptides activate growth or repair mechanisms in the body, raising theoretical risks of unwanted cell proliferation that cannot be ruled out without rigorous trials.
Even when purchased from seemingly reputable clinics, the substances do not carry the safety guarantees associated with FDA-approved medications. There are no standardized dosing guidelines, no adverse event reporting systems, and no established monitoring procedures for patients. For regulators and medical professionals, this creates a situation where thousands of individuals are effectively participating in an uncontrolled experiment without the safeguards normally required for drugs injected directly into the bloodstream.
Political and Cultural Dimension
The peptide-stacking phenomenon is not emerging in a political vacuum. It has been amplified by public figures who frame it as part of a larger struggle against federal regulation. Robert F. Kennedy Jr., through his “Make America Healthy Again” effort, has positioned peptides as an example of therapeutic freedom and has criticized the FDA for restricting their use. Kennedy has promoted peptides on social media and at campaign-style events, even though many of the compounds he references lack approval and have never been tested in controlled human trials.
This rhetoric taps into a broader movement that views federal oversight as an obstacle to personal autonomy. Several peptide advocates echoed Kennedy’s arguments and claimed that individuals should have the right to inject whichever compounds they choose, regardless of regulatory warnings. This approach treats peptides less like experimental drugs and more like lifestyle choices, which complicates public health messaging and undermines the FDA’s ability to intervene when unsafe products proliferate.
At the same time, the administration’s posture toward medical science has contributed to the public confusion surrounding these substances. While Trump has aggressively promoted efforts to reduce the cost of GLP-1 weight-loss drugs, his political allies continue attacking vaccines and other well-established medical treatments. This divided stance fosters an environment where untested alternatives gain legitimacy while proven interventions come under unwarranted scrutiny.
Culturally, peptides have gained traction by aligning with the aesthetics of modern biohacking and longevity culture. Social media influencers frequently present peptide injections as a futuristic upgrade to wellness routines, similar to cold plunges, IV drips, and nootropic supplements. This appeal is often aspirational; users hope peptides offer a shortcut to athleticism, youth, or enhanced metabolism, especially in an era where anti-aging narratives dominate online health communities.
These broader dynamics create a powerful mix of political distrust, scientific misunderstanding, and cultural aspiration. Together, they form the conditions under which a largely unregulated practice can flourish. The result is a marketplace where unproven compounds are promoted as revolutionary breakthroughs while the scientific process designed to protect public safety is cast as an impediment rather than a safeguard.
Is There Science Behind It (or Not)?
Although peptides play legitimate roles in medicine, the specific compounds driving the stacking trend generally do not have human trial data to support their advertised benefits. While some therapeutic peptides, such as insulin, are rigorously tested and regulated, the peptides now spreading across wellness culture exist in a scientific vacuum. Many have been studied only in animals, and in some cases only in isolated biochemical experiments, which makes the claims circulating online difficult to evaluate through any evidence-based framework.
The scientific gap becomes even wider when these substances are combined. Stacking involves injecting multiple peptides with overlapping or ambiguous biological pathways, yet there is no research demonstrating how these compounds interact inside the human body. Reporting on the peptide boom notes that none of the most popular wellness peptides have undergone controlled trials examining how they behave when paired together, which leaves both efficacy and safety unresolved. Without data on synergistic or antagonistic effects, clinicians cannot reliably predict outcomes.
Researchers have also raised concerns about the mismatch between marketing and evidence. Several peptides promoted for fat loss, muscle recovery, or anti-aging effects are supported only by early animal studies. Animal models cannot determine human dosing, long-term metabolic effects, or cancer risks linked to artificially stimulating growth-related pathways. This is especially relevant for compounds like BPC-157 and TB-500, which are heavily marketed online despite a lack of validated human research.
Medical experts warn that even seemingly benign peptides may carry hidden risks. Without controlled trials, clinicians cannot assess how the body metabolizes these compounds over time, whether they accumulate in tissues, or whether chronic use could produce unintended hormonal or immune effects. Experts interviewed by NBC News emphasized that purity and potency vary widely among unregulated products, which only deepens the scientific uncertainty.
The absence of research does not mean peptides are inherently harmful, but it does mean their safety and benefits remain unproven. Scientists agree that meaningful human studies are required before these substances can be responsibly recommended. Until such trials exist, peptide stacking remains closer to self-directed experimentation than legitimate medical treatment, leaving consumers exposed to risks that science has not yet begun to quantify.
Risks, Warnings, and Clinical Advice
Medical experts have issued increasingly direct warnings about the dangers of peptide stacking as the trend spreads. Physician and researcher Eric Topol described the practice as “really dangerous” precisely because none of the products being injected by consumers have undergone the clinical testing required to determine safety. He emphasized that the compounds sold online are unapproved drugs, not supplements, and that their effects on humans remain unknown in structured scientific terms. This absence of validated information makes it impossible to determine safe dosing, appropriate duration of use, or even whether certain peptides should be injected at all.
Concerns extend beyond the peptides themselves to the way they are produced and distributed. Many vials were manufactured in unregulated facilities and sold without quality control standards that govern legitimate pharmaceuticals. Wellness clinics and online sellers rarely disclose where their products come from or whether they have been tested for sterility. Without assurances regarding purity or concentration, consumers may be injecting compounds contaminated with bacteria, heavy metals, or incorrect peptide levels, risks that would normally be mitigated by FDA oversight.
Clinicians have stressed that the lack of established dosing guidelines significantly increases the potential for harm. Because no clinical trials exist, practitioners cannot rely on evidence-based frameworks to guide patient use, and many of the individuals injecting peptides are doing so based on online tutorials rather than medical supervision. This creates opportunities for overuse, unsafe combinations, and interactions with existing medications, none of which can be adequately assessed in the absence of controlled human research.
Public health experts argue that consumers should be cautious and consult qualified medical professionals before considering any peptide product. They note that while peptides have legitimate therapeutic applications in regulated medical contexts, the compounds circulating in wellness communities do not fall into that category. Until human trials establish safety and efficacy, clinicians recommend avoiding unapproved injections altogether and relying instead on treatments that have undergone the rigorous testing required to protect patient health.
Broader Implications and Questions
The rapid spread of peptide stacking raises significant public health questions. Because these compounds are unapproved drugs, there is no federal system in place to monitor adverse reactions, track complications, or collect long-term outcome data. Users often share their experiences only through social media communities, which means that potential harms may never reach clinicians or regulators. Without structured reporting channels, health officials cannot evaluate whether widespread peptide use is producing patterns of injury or other medical concerns.
Legal and ethical issues also shape the debate. Many peptides are marketed with “research use only” labels even though they are clearly intended for consumer injection. This creates a loophole where companies can sell drug-like substances while avoiding the regulatory responsibilities associated with pharmaceuticals. Consumers may interpret the availability of these products as evidence of legitimacy, even though the sellers themselves avoid making explicit medical claims in order to stay outside FDA jurisdiction.
Industry behavior adds to the complexity. The popularity of legitimate GLP-1 weight-loss medications has driven consumer interest in anything described as a “peptide,” regardless of whether the product has undergone scientific scrutiny. This dynamic blurs the line between regulated medicine and speculative biohacking, creating a marketplace where branding often matters more than evidence. It also encourages manufacturers to push out new compounds quickly in response to demand, sometimes without verifying purity or consistency.
The long-term cultural implications remain uncertain. If peptide stacking continues to expand, regulators may be forced to choose between cracking down on gray-market sellers or developing new pathways to evaluate emerging compounds. Scientists agree that rigorous human research will be essential if peptides are ever to transition from fringe wellness products to legitimate therapies. Until then, the trend highlights the tension between consumer desire for personalized enhancement and the safeguards required to ensure medical safety.
Conclusion
Peptide stacking has emerged as one of the most visible examples of the widening divide between scientific evidence and wellness culture. Despite the bold claims circulating on social media and in boutique clinics, reporting all points to the same reality: these substances have not been tested in humans, have not been approved by the Food and Drug Administration, and remain virtually unregulated in both manufacturing and distribution. The gap between the hype and the available evidence is not merely a scientific concern; it is a public health issue.
The political environment surrounding the trend has only intensified the confusion. As public figures like Robert F. Kennedy Jr. champion peptides as part of a broader challenge to federal oversight, the market for untested compounds grows alongside ongoing skepticism toward proven medical treatments. Meanwhile, the administration’s emphasis on lowering costs for GLP-1 medications underscores how legitimate and well-studied therapies can coexist uneasily with a booming gray market of unapproved injections. Consumers are left navigating mixed messages as marketing outpaces scientific validation.
Ultimately, the future of peptides depends on evidence, not enthusiasm. Scientists stress that rigorous human trials are the only way to determine whether these compounds have therapeutic value or pose meaningful risks. Until that research exists, peptide stacking remains an uncontrolled experiment conducted on the public, marketed with the aesthetics of innovation but lacking the safeguards that define modern medicine. The question moving forward is whether regulators, clinicians, and consumers will demand evidence before the next phase of this trend takes hold.
Originally published by Brewminate, 11.20.2025, under the terms of a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International license.


