How masks were actually used in the military in 1918 and how their effectiveness was evaluated in contemporary reports.

By Dr. E. Thomas Ewing
Professor of History
Virginia Tech

By Jessica Brabble
Graduate Student in History
Virginia Tech

By Dr. Ariel Ludwig
HPE Data Institute
University of Houston

By Dr. Linsey C. Marr
Charles P. Lunsford Professor of Civil and Environmental Engineering
Virginia Tech

By Katherine Randall
Doctoral Candidate, Rhetoric and Writing
Virginia Tech
During the 1918 influenza epidemic, the US military responded to infectious disease outbreaks with preventive or containment measures including isolation wards, masks, improved sanitation, health checks, and quarantine requirements. The use of masks was documented in photographs of patients, nurses, and doctors and the effectiveness of masks was evaluated in studies published after war.

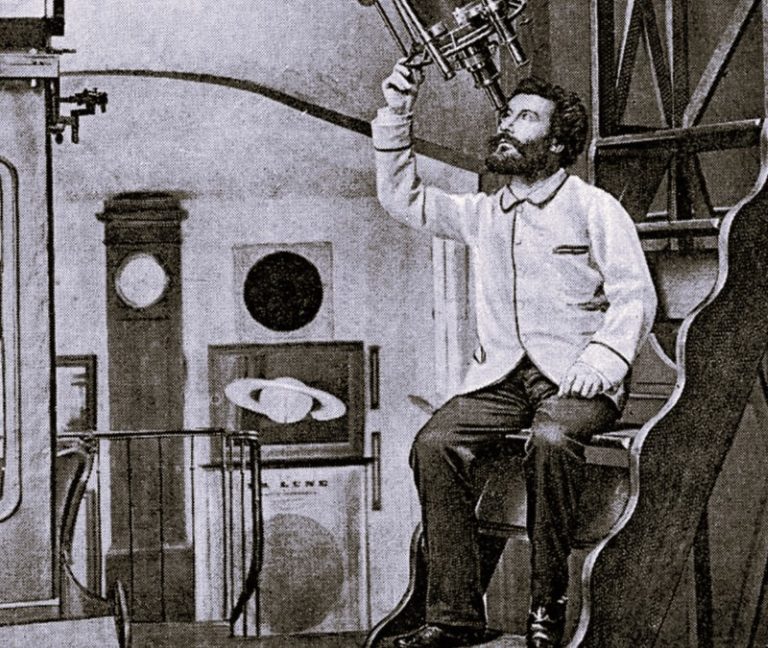
A photograph from Base Hospital No. 82, Toul, France, shows two women and four men wearing masks (Illustration 1). Although undated, the photograph was likely from October 1918, when this hospital treated more than five hundred patients with acute respiratory infections. A closer look at the photograph, however, reveals that all of the masks were worn incorrectly, as noses were not fully covered. Photographs like these provide evidence of the differences between theory and practice and help us better understand how the imperfect implementation of masks as a public health measure made judging their effectiveness after the fact difficult.

All together, we looked at fifteen photographs from a dozen hospitals that depict actual mask use. Of the 87 people (65 patients and 22 medical staff) in the photographs, 16% are wearing masks correctly, 5% are wearing masks incorrectly, and 79% are not wearing masks at all. Medical staff were more likely to wear masks: 36% of nurses, doctors, and orderlies wore masks, as compared to just 9% of patients (chart 1). Given all that we have learned in the past year about how masks prevent infection, the relative absence of masks during the 1918 epidemic is quite striking.

This evidence of inconsistency in mask behavior partially explains the mixed conclusions regarding mask effectiveness in US military reports following the epidemic. The authoritative history, The Medical Department of the United States Army in the World War introduces the section, “Use of the Mask,” by acknowledging that the “value of face masks worn by the whole of a command has been the subject of much argument.” (p.118) While it “appears to be generally conceded that the use of the mask by attendants on the sick, exposed constantly to infection, is of value,” the study called attention to the fact that “attendants, especially nurses,” were disproportionately “attacked,” even though they regularly wore masks. The report offers an ambivalent recommendation about masks in medical facilities: “Under these circumstances judgment as to the value of the mask becomes difficult.”
A review of mask mandates for camps and bases leads to even more equivocal conclusions. Statistics from US facilities found that 51% of 41 camps using masks and 52% of 77 camps not using masks reported above average rates of influenza, leading to this assessment after the war:
“It is evident that the mask may be an efficient means of limiting the spread of infection. It is equally evident that unless the necessary conditions are fulfilled in the construction and wearing of the mask it may be useless…. For this reason, statistics as to the results attained in the general use of the mask in Army camps during the epidemic are of doubtful value.” (pp.119-120)
Yet the report also conceded that “no one has expressed the opinion that the mask properly used can do harm,” while “experimental evidence points to the probability of its usefulness.” The title of this essay is derived from this report’s strikingly ambivalent determination that “the mask is probably of great value potentially.” (pp.119-120)
The Annual Report of the Surgeon General of the US Navy reached the even more critical conclusion that wearing masks was “not a practicable measure and little or no good was accomplished.” (p. 433) The concerns began with the design but also included criticism about behaviors that compromised their effectiveness:
“Masks of improper design, made of wide-mesh gauze, which rest against the mouth and nose, become wet with saliva, soiled with the fingers, and are changed infrequently, may lead to infection rather than prevent it, especially when worn by persons who have not even a rudimentary knowledge of the modes of transmission of the causative agents of communicable disease.” (p. 434)
Although “on theoretical grounds it is good practice to require those who visit, examine, or wait upon the sick to wear masks,” results from medical facilities were not conclusive. At the Naval Training Station at Great Lakes, Illinois, only 14% of medical staff wore masks, yet their infection rate of 8.3% was higher than the 7.9% rate for those not wearing masks. The Navy Surgeon General report concluded that “the use of masks in barracks is not a practicable measure of value under ordinary routine conditions” and thus recommended against “compelling persons at large to wear masks during an epidemic.” (p. 434)
While these broad surveys were unable to find conclusive evidence about mask effectiveness, reports at the local level tended to credit masks along with other measures for controlling the disease. At Base Hospital No. 58, according to the Army Surgeon General’s Annual Report, all patients were “masked upon admittance” and required to “wear masks as long as sick in the hospital.” This measure, along with isolating infectious disease cases and practicing good hygiene, was credited with keeping infection rates low. At Base Hospital No. 80, “the cubical [sic] and mask system of handling all respiratory cases as well as contagious cases was installed as soon as we began receiving patients, and a good deal of the credit must be given to this measure for the good results obtained.” (pp. 1998-1989) At the Philadelphia Navy Yard, where the medical officer “ordered that gauze masks be made and distributed among the yard employees,” the Navy Surgeon General’s report concluded that “there is good reason to believe that this procedure contributed largely to the preservation of the health of the employees, as not one department or portion of a department in the yard was forced to slacken its work in the least.” (p. 300)
These photographs and reports indicate that the use of masks during the 1918 epidemic was neither universally practiced nor uniformly evaluated. By contrast, public health experts in 2020-2021 have consistently endorsed the use of masks and mask mandates have been widely imposed, although these measures have been publicly contested and occasionally disregarded. Evidence from the 1918 epidemic leads to three conclusions: first, the main challenge is explaining why this change in behavior is so vital to protecting the health of all; second, understanding how masks work to filter droplets and aerosols can be persuasive for individuals and policy-makers; and third, masks will not work if they are not worn correctly and consistently. The cognitive dissonance we feel when looking at photographs of unmasked patients and staff in infectious disease wards a century ago is a reminder of why we now choose to wear masks in any situation with the potential for infection.
Originally published by the U.S. National Library of Medicine, 04.22.2021, to the public domain.