
The vaccines will be remembered as a triumph of science.

By Matthew A. McIntosh
Public Historian
Brewminate
Introduction
The COVID-19 pandemic emerged as one of the deadliest and most disruptive global events since the 1918 influenza pandemic. As governments, healthcare systems, and societies struggled to manage the devastating spread of SARS-CoV-2, the global race to develop an effective vaccine unfolded with unprecedented urgency. The deployment of COVID-19 vaccines in late 2020 and throughout 2021 marked a turning point in the battle against the virus. Mounting scientific evidence, epidemiological modeling, and real-world data demonstrate that these vaccines saved millions of lives globally, transforming the trajectory of the pandemic.
Development and Distribution
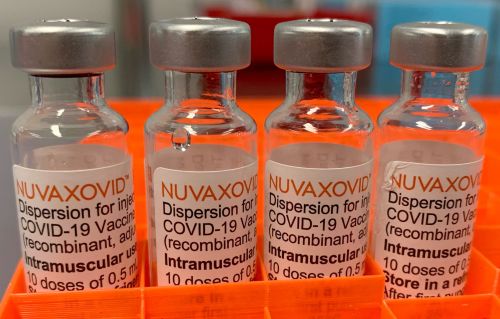
The rapid development of COVID-19 vaccines was made possible through decades of prior research in virology, immunology, and vaccine technology. Notably, mRNA technology, long in development but previously unproven on a large scale, became a leading tool in the pandemic response. Pfizer-BioNTech and Moderna were the first to deliver mRNA-based vaccines that demonstrated over 90% efficacy in preventing symptomatic COVID-19 in clinical trials.1
What made this rollout extraordinary was the speed and coordination between governments and private pharmaceutical companies. Initiatives like Operation Warp Speed in the United States enabled accelerated development, regulatory review, and production. The global COVAX initiative aimed to provide equitable vaccine access to low- and middle-income countries, although distribution disparities remained a challenge.2
Life-Saving Impact: Modeling the Data
Several studies and statistical models have sought to quantify the impact of vaccines in preventing deaths. A landmark study published in The Lancet Infectious Diseases in 2022 estimated that COVID-19 vaccines prevented over 20 million deaths globally in the first year of availability.3 This study utilized data from 185 countries and territories, applying excess mortality and reported COVID-19 death data to model vaccine impact under counterfactual scenarios.
In the United States alone, the Centers for Disease Control and Prevention (CDC) estimated that vaccination prevented more than 1 million deaths, 10 million hospitalizations, and 36 million infections from December 2020 through November 2022.4 Similar trends were reported in the United Kingdom, Canada, and several European countries, highlighting the global relevance of immunization efforts.
Reduction in Severe Outcomes
Beyond mortality, vaccines played a crucial role in reducing hospitalizations, long-term complications, and healthcare burden. Research consistently demonstrated that even during the emergence of new variants such as Delta and Omicron, vaccines retained strong efficacy in preventing severe outcomes.5 While breakthrough infections did occur, particularly as new variants evolved, vaccinated individuals overwhelmingly experienced milder symptoms and recovered more quickly than their unvaccinated counterparts.
Booster doses further enhanced protection, especially among high-risk populations such as the elderly, immunocompromised, and frontline workers.6 This layered approach to vaccination – initial series followed by booster shots – exemplified how adaptive vaccine strategies could be implemented in real time based on emerging data.
Debunking Myths
One of the most persistent and dangerous narratives surrounding COVID-19 vaccines has been the assertion that they were harmful or even deadly. However, overwhelming scientific consensus, based on rigorous monitoring and data collection, refutes this claim. The most comprehensive safety monitoring in vaccine history was undertaken through systems such as the CDC’s Vaccine Adverse Event Reporting System (VAERS), the FDA’s Biologics Effectiveness and Safety (BEST) initiative, and international pharmacovigilance efforts.7
While mild and temporary side effects—such as soreness at the injection site, fatigue, or low-grade fever—were common and expected, serious adverse events were extremely rare. For example, myocarditis following mRNA vaccination occurred in approximately 12.6 cases per million second doses in young males—rates significantly lower than myocarditis caused by actual COVID-19 infection.8 Independent reviews consistently concluded that the benefits of vaccination far outweighed the minuscule risks.
Claims that the vaccine caused widespread death are demonstrably false. A detailed study in Nature Communications examined mortality data across several nations and found no increase in all-cause mortality following vaccination, confirming the absence of any deadly vaccine-induced trends.9 Additionally, misinterpretations of VAERS data—often cited in misinformation campaigns—were frequently debunked by the CDC and public health experts, who emphasized that reports in VAERS do not establish causation.10
Moreover, global trends showed that as vaccine coverage increased, hospitalization and death rates fell dramatically, even during subsequent waves of infection. If vaccines were harmful on the scale alleged by conspiracy theorists, these patterns would not be consistent. Instead, the evidence clearly showed that vaccines were the primary driver of reduced COVID-19 mortality.
Vaccination and Public Health Equity
Although the vaccines had tremendous success in high-income countries, their distribution revealed stark global health inequities. While nations such as the U.S., U.K., and members of the European Union secured large vaccine supplies early on, many low-income countries struggled to access sufficient doses. As of late 2022, less than 25% of people in low-income countries had received at least one vaccine dose.11
This disparity not only raised ethical concerns but also had practical implications. Continued transmission in unvaccinated populations increased the likelihood of new variant emergence. International health organizations and humanitarian groups called for a reevaluation of global health governance and funding mechanisms to better prepare for future pandemics.
Combating Misinformation
The vaccine rollout also encountered significant resistance due to misinformation and politicization. Social media played a central role in spreading unfounded fears about vaccine safety, fertility impacts, and government control.12 Despite overwhelming scientific consensus on the safety and efficacy of vaccines, public health campaigns often struggled to reach skeptical communities.
In some regions, vaccine hesitancy materially affected uptake rates, prolonging the burden of COVID-19. However, many grassroots efforts involving community leaders, healthcare providers, and educators helped counter these narratives and promote vaccine confidence.13 The experience highlighted the need for improved science communication and trust-building in public health systems.
A Lasting Legacy
The success of the COVID-19 vaccine campaign stands as a historic achievement in medicine and global cooperation. It not only averted millions of deaths but also demonstrated the power of innovation and collective action. The crisis accelerated advancements in mRNA technology, pandemic surveillance, and global health infrastructure, leaving a lasting legacy that extends beyond COVID-19.
As future generations reflect on the pandemic, the vaccines will be remembered as a triumph of science in the face of unprecedented adversity. The lessons learned underscore the need for sustained investment in public health, equitable access to medical innovations, and global solidarity in confronting emerging threats.
Endnotes
- Katalin Karikó and Drew Weissman, “mRNA Therapeutics: A New Era in Vaccine Technology,” Nature Reviews Drug Discovery 19, no. 5 (2020): 273–274.
- World Health Organization, “COVAX: Ensuring Global Access to COVID-19 Vaccines,” WHO.int, accessed April 10, 2023, https://www.who.int/initiatives/act-accelerator/covax.
- Oliver J. Watson et al., “Global Impact of the First Year of COVID-19 Vaccination: A Mathematical Modelling Study,” The Lancet Infectious Diseases 22, no. 9 (2022): 1293–1302.
- Centers for Disease Control and Prevention, “COVID-19 Vaccine Impact Estimates,” CDC.gov, last modified December 2022, https://www.cdc.gov/vaccines/covid-19/effectiveness-research.html.
- John M. McLaughlin et al., “Clinical Effectiveness of COVID-19 Vaccination Against Severe Outcomes with Delta and Omicron Variants,” JAMA 328, no. 6 (2022): 546–555.
- Ziyad Al-Aly et al., “Protection and Waning of Natural and Hybrid Immunity to SARS-CoV-2,” Nature Reviews Immunology 23, no. 1 (2023): 15–28.
- U.S. Food and Drug Administration, “FDA’s BEST Initiative,” FDA.gov, accessed January 2023, https://www.fda.gov/drugs/surveillance/fdas-best-initiative.
- Matthew E. Oster et al., “Myocarditis Cases Reported After mRNA-Based COVID-19 Vaccination in the US From December 2020 to August 2021,” JAMA 327, no. 4 (2022): 331–340.
- Daniel M. Weinberger et al., “Estimation of Excess Mortality Associated With COVID-19 by Age and Sex in 19 Countries, 2020–2021,” Nature Communications 14, no. 1 (2023): 1510.
- Centers for Disease Control and Prevention, “VAERS Frequently Asked Questions,” CDC.gov, accessed November 2022, https://vaers.hhs.gov/faq.html.
- Our World in Data, “COVID-19 Vaccine Doses Administered by Country,” OurWorldInData.org, accessed December 1, 2022, https://ourworldindata.org/covid-vaccinations.
- Center for Countering Digital Hate, “The Disinformation Dozen,” CCDH.org, March 2021, https://www.counterhate.com/disinformationdozen.
- Monica Schoch-Spana et al., “Building Trust in COVID-19 Vaccines through Community Engagement,” Health Security 19, no. 4 (2021): 309–316.
Originally published by Brewminate, 05.30.2025, under the terms of a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International license.


