By Joseph A. Legan
Introduction
The Black Death pandemic of the 14th century is one of the most well-known and studied disease outbreaks in history. The pestilence caused by the bacteria Yersinia Pestis likely originated in the Mongolian steppes around 1331. By 1353, the Plague had spread throughout most of Europe, Asia and North Africa, with mortality rates as high as 75% in some areas. Medical professionals in both the Middle East[1] and Europe were woefully unprepared to handle an epidemic of this magnitude. Physicians at the time were reliant on medical techniques and theories that dated back to Aristotle and Hippocrates in the 4th century BCE. Though many did try, doctors had no real way to cure or prevent the disease. Along with religious causes, medical causes, such as theories of humors and the spread of pestilential miasmas, were put forth to explain the Plague. Even though medicine in the Middle East was marginally more advanced than European medicine, particularly in the areas of surgery and anatomy, physicians in both regions were unsuccessful at treating the Plague; however, the Black Death served to promote medical innovations that laid the foundations of modern medicine.[2]
Biomedical Context
The Black Death was caused by a complex series of bacterial strands collectively known as Yersinia pestis. The bacteria normally live in the digestive tract of the rat fleas Xenopsylla cheopis and Cortophylus fasciatus, but it can also live in the human flea, Pulex irritans. The bacteria multiply in the flea’s stomach rapidly enough to cause a blockage, which threatens the flea with starvation. While feeding, the flea then regurgitates some of the bacteria into its victim. Y. pestis can only pass through a break in the skin; it cannot pass through healthy skin.[3]
Many rodents can carry the Plague, including tarbagons, marmots, and susliks in Asia. In Europe, the main carrier of the Plague was the black rat, Rattus rattus, though virtually every household and barnyard animal could also carry the Plague, except for horses, whose odor repels fleas. The fleas infected with Y. pestis generally only bit humans once they ran out of other hosts. In other words, humans were not the preferred host of Y. pestis, they were victims of an animal epizootic disease.[4]
The rat flea X. cheopis can survive for up to a year without a rodent host. However, the flea is only active at temperatures between 15 and 20 ̊C (59 and 68 ̊F) with humidity between 90% and 95%. The flea will die if the humidity drops below 70%. This explains why the Plague was generally the most lethal in late summer and early spring in Western Europe; that was when climatic conditions were the most ideal for the fleas. Additionally, when the rodent population was large enough, it formed a reservoir for the Plague. Once all the rodents died out, Y. pestis was able to survive in the dark moist environment of rodent burrows for an extended amount of time. If a new rodent population moved in, they would become infected, and a new epidemic would begin. This explains the cyclical occurrence of the Plague after the initial epidemic in the 14th century. The Plague would not strike as a single epidemic, but as a pandemic, which is a linked series of epidemics occurring in a cyclical fashion. The frequency of the disease made the Black Death deadlier than its virulence alone.[5]
There were three main varieties of the Plague: bubonic, pneumonic, and septicaemic. Bubonic was the most common form of the plague. It had an incubation period of approximately six days. Initially, a blackish gangrenous pustule would appear at the sight of the bite, followed by a swelling of the lymph nodes in the armpits, groin, or neck, depending on the location of the bite. Next, subcutaneous hemorrhaging occurred, causing swelling and purplish blotches in the lymphatic glands. These blotches were known as buboes, which is the namesake of the Plague variant. The hemorrhaging caused cell neurosis and intoxication of the nervous system, leading to neurological and psychological disorders.[6] Diarrhea, vomiting, and pneumonia sometimes accompanied bubonic plague.[7] The bubonic form was the least lethal of the three forms, but it still killed between 50% and 60% of its victims.[8]
Pneumonic plague was the only Plague variant that could be transmitted directly from person to person. It occurred when the infection moved into the lungs. After an incubation period of between two and three days, body temperature dropped, followed by a severe cough, consolidation in the lungs, and the discharge of bloody sputum. The sputum contained Y. pestis. Neurological difficulties and coma followed infection, which resulted in death to 95 to 100% of victims.[9]
Septicaemic plague was the rarest and most lethal form of the Plague. It was always fatal.[10] Like the Bubonic form, it was transmitted by insects, not from person to person. Septicaemic Plague occurred when the bloodstream became infected. The blood became swarmed with bacteria within several hours. The victim died before buboes could even form. There were enough bacteria in a victim’s bloodstream that if an uninfected flea bit them, the flea would become infected and then could spread the Plague. This is the primary way that the human flea, P. irritans, infected other humans with the Plague.[11]
There were two pandemics of the Black Death in medieval Europe. The first epidemic of the first pandemic occurred in 541 CE and was known as Justinian’s Plague. At the time, the Byzantine Emperor Justinian was trying to reconquer the areas of the Western Roman Empire that were under control of the Germanic warlords. Roughly 40% of Constantinople’s population perished as did 25% of Europe’s population south of the Alps. The Pestilence crippled Justinian’s plans to retake Western Europe and arguably weakened Byzantium enough to be overwhelmed by the Arabs a few generations later. Subsequent epidemics occurred every 10 to 24 years during the next 200 years. The overall population loss from 541 to 700 is estimated to be about 50%. After the 8thcentury, the Plague did not strike the whole of Europe until 1346.[12]
Between the 10th and 14th centuries, the population of Europe increased by 300% up to 80 million, the highest the population had been for a thousand years.[13] Warm weather and adequate moisture in the 13th century along with the lack of any epidemic fueled the population boom.[14] The Crusades provided an outlet for belligerent tendencies, so Europe itself was relatively peaceful.[15] The Christian West had expanded its borders to Russia and the Middle East. Internal trade within Europe improved considerably with new Alpine passages and sea routes. International trade between Europe, Asia, and Africa also greatly increased. The rising population and increase in trade greatly increased the probability for a new pandemic of the Black Death by the 14th century.[16]
The Black Death in Europe
The Black Death originated in the East, likely in the Mongolian steppes. Historians are sure that the nomadic Mongolian Empire helped spread the Plague, but they are divided between two theories of how it occurred. The first theory, developed primarily by William McNeill, states that by the end of the 13thcentury, the Mongols had reached the Yunan region in southern China, which is today an inveterate focus of the plague. The Mongols brought the Plague causing bacteria, Y. pestis, with them back to their capital in the Gobi Desert, Karakorum. From there, it spread throughout the empire and eventually reached Europe.[17] The second theory, the environmental theory, claims that wind patterns changed in Asia, resulting in hot, dry Saharan air being blown into the already dry central Asia. The Mongol and Turkic nomads were then forced to move their flocks east and west in search of greener pastures. Likewise, the central Asian rodent population was forced to migrate. Both the movement of the flocks and the rodents spread the plague.[18]

The Plague spread westward both by the movement of infected animals and by the movement of men via the elaborate east-west trading system established in the 12thand 13thcenturies. Under Mongol rule, caravans were guaranteed protection, which resulted in the reinvigoration of the Silk Road. At the end of these trade routes emanating from east and south Asia were Italian merchants, mainly Genoese, Venetians, and Pisans. They brought various goods from eastern Mediterranean and Black Sea ports back to Italy and southern France. From 11there, the goods were taken overland into northern Europe. Y. pestis could be carried by fleas and rats aboard the ships,or by the merchants themselves (Figure 1).[19]
Traditionally, the first documented case of the Black Death in Europe is said to be at the Genoese settlement of Caffa on the Crimean Peninsula in September 1346. The lawyer Gabriel de’ Mussis described that in 1346, “countless numbers of Tartars and Saracens were struck down by a mysterious illness.” He also mentioned how the Tartar army fell ill while invading Caffa.The Tartars died by the thousands, but they launched the dead bodies over the city walls, and soon, the Genoese were infected.[20]
The Plague then spread to Constantinople, the capital of the Byzantine Empire, and one of the largest Christian cities in the world, with a population of well over 100,000.[21] Emperor John VI Cantacuzenos documented the Plague in Constantinople. Though not trained in medicine, he was educated in Greek literature, and knew of a description of the ancient Athenian Plague in Thucydides’ History.[22] The emperor’s son, Andronikos, was infected with the Plague and died within three days. In Cantacuzenos’ description, he tells of how the Plague started with the Hyperborean Scythians, of Southern Russia, and spread through Pontus, Thrace, Macedonia, Greece, Italy, and throughout the entire world. In his account, he also discusses the symptoms of the plague: “sputum suffused with blood was brought up,” “black blisters appeared,” and “some people broke out with black spots all over their bodies.” He also notes how those few who survived the sickness were never infected with it twice.[23] Venetian ships visiting Constantinople spread the Plague throughout the Venetian territory along the Balkans by December of 1347 or January 1348. From there, it spread eastward into the Kingdom of Hungary.[24]
The Franciscan monk, Michele da Piazza describes the arrival of the Plague to Sicily. In October 1347, 12 Genoese galleys arrived in Messina. The Genoese on board “carried such a disease in their bodies that if anyone so much as spoke with one of them he was infected with a deadly illness and could not avoid death.” Once the people of Messina realized the sickness came from the Genoese, they expelled them from the city. However, it was to no avail, “The illness remained in the city and subsequently caused enormous mortality.”[25] From Sicily, the Plague was brought into mainland Italy by the end of the year via Pisa and Genoa, both of which suffered between a 30% and 40% drop in population.[26] More than 70% of those infected with the Plague died, and quickly, 20 out of the 24 physicians in the city perished as well.[27] From there, the Plague spread throughout Tuscany, Italy’s most prosperous and industrialized region. Scholarly estimates for the morbidity rate of Florencerange from 45% to a high of 75% of the total population.[28] The Plague hit Italy so hard that slavery was briefly reintroduced to make up for the unprecedented labor shortage.[29]
From Italy, the Plague spread across the western Mediterranean basin. It reached Marseilles, a principal French port, by January 1348. Mortality among the southern French cities averaged around 40%. Avignon, the seat of the Papacy, was hit by the Plague in early 1348 as well. As many as one third of the cardinals perished, and Pope Clement VI, at the advice of his physician, fled the city until the plague had subsided.[30]
The Black Death penetrated Iberia from at least three different entry points. Plague initially came from the south, across the Straits of Gibraltar, from the Moorish caliphates of North Africa to those of Southern Iberia. Second, it crossed the Pyrenees in the north and infected the Basque region. Lastly, it was transported to the Balearic Islands by Italian merchants, and then was brought to the major ports of eastern Spain, including Barcelona and Valencia, where between 30% and 40% of the population died. Gibraltar itself was one of the last places in Iberia to be infected by the Plague; the first reported case was not until the spring of 1348. In 1350, while the Muslim Granadan fortress at Gibraltar was besieged by the Christian Castilian army, Plague broke out on both sides. King Alfonso XI of Castile refused to end the siege, and became ill and died in March. He was the only European monarch to have died from the Plague. By the end of 1350, the Plague had struck the entire Mediterranean basin and killed between 35% and 40% of its population.[31]
From southern France, the Plague spread northward via the Rhone River valley and other land routes. At the time, France was the most populous Christian kingdom with a population between 18 and 24 million. The Plague hit Paris, the largest city in northern Europe, with a population somewhere between 80,000 and 200,000, in the summer of 1348. At its peak in late fall and early winter, it was reported that 800 people died every day.[32] Contemporary reports claimed that someone who was healthy one day could end up dead and buried the next day.[33] From France, the Black Death spread northward into Picardy and the Low Countries. It hit the rural Netherlands relatively lightly, only between 20% and 25% of its population died, which was no more severe than the great famines of the 1310s.[34]

Most contemporary writers say Melcombe Regis, modern day Weymouth, was the point of entry for the Plague into England in July or August 1348. It probably entered England through English cities in France, such as Calais. From the southwest, it spread to Bristol, then Oxford, and then finally to London. It likely reached London in October or November, though it was not officially recognized by Parliament until January. Despite the fact that the Plague normally dissipated in winter months, there is evidence that suggests it was highly active in England during the winter of 1348/1349. The winter was unusually warm and wet, allowing favorable conditions for fleas. There were a high number of vacant benefices in the diocese of Salisbury during the fall and winter likely caused by the death of their incumbents by the Plague.[35]
The Plague was most severe in the spring of 1349. From February 2 to April 2, an average of 290 deaths occurred every day in London.[36] It is estimated that between twenty and thirty thousand Londoners perished, out of a total population of between sixty and seventy thousand. The existing graveyards were quickly filled and new ones had to be open to meet the demand. Both the poor and the powerful were struck down by the Plague. Three Archbishops of Canterbury died between 1348 and 1349: John Stratford, John Offord, and Thomas Bradwardine. The Black Deathevenreached the royal family; King Edward III’s daughter, Joan, died from the Plague. The King even discontinued the session of Parliament in January 1349.[37] One English author states that to offer comfort to those who were dying, the Pope granted plenary remission of all sins at the point of death until Easter of 1349.[38]
From London, the Black Death spread northward into East Anglia and then to the Midlands and into Wales[39] where it drastically reduced the price of rents. The Plague arrived in Ireland as early as spring 1349 via ships originating from Bristol and Chester.[40] The pestilence killed many people and hit the kingdom of Magh Luirg particularly hard.[41] Mortality rates peaked during the summer when it killed the archbishop of Dublin, the most important churchman in Ireland.[42] Once the Scots heard of the pestilence in England, they believed that it was the result of an avenging God. While readying their forces to invade England, the Plague struck them and their army was decimated.[43] Even though Scottish contemporary writers claimed the Pestilence killed a third of the world’s population, modern historians are certain the incidence of the Plague in Scotland was uneven because Plague carrying rats did not find ideal conditions for colonization among the Scottish highlands, and the density of R. rattus correlated with the intensity of the Plague. Most contemporary sources claimed the Plague spread to Scotland across the English border, this is not likely true due to the fact that the English and Scottish were at war; therefore there was little trade between them. Plague likely came from the continent aboard merchant ships.[44]
The Black Death entered the Far North through the Norwegian port of Bergen in May 1349. Bergen was one of the largest cities in Scandinavia, and a major port in the Hanseatic League. That month, an English wool ship was drifting around the harbor. Plague had struck the ship and killed everyone aboard. Once it ran aground, it was boarded by municipal authorities, who unintentionally spread the Plague to Bergen. By the end of 1350, it had spread all throughout Scandinavia and killed roughly half of the population.[45] Historians have been divided on whether the Plague reached Iceland; however, Icelandic annals flatly state that the Black Death never reached Iceland. In addition to Iceland, evidence suggests that the Black Death did not reach Finland during the 14thcentury. There are two factors that explain this. The first is that population density in Finland at the time was incredibly low; the total population was significantly less than 100,000 people spread out across the large area. In addition, the Plague likely hit Sweden so hard that trade across the Baltic Sea halted.[46]
The Black Death invaded Austria through the Brenner Pass from Italy in July 1348.[47] In Neuberg, goods bequeathed by the dead were not accepted out of fear that they carried the Plague that killed their previous owners.[48] The Black Death entered Germany both across the Alps from Austria and across the Rhine River from France and the Netherlands. The mortality rates in Germany were much lower than in the Mediterranean Basin, the British Isles, and Scandinavia. The highest rates only approached 30% in Baltic cities such as Bremen and Hamburg; the lowest rates were a mere 10% in Alsace and Lorraine. However, hysteria due to the Plague resulted in widespread persecution of Jews as well as widespread flagellism throughout Germany, two phenomena closely identified with the Black Death.[49]
Poland is traditionally thought to have escaped the Plague; however this theory is possibly untrue. Areas that are in present day Poland, such as Prussia and Pomerania were certainly struck by the Plague, and it is possible that the Plague was able to spread down the Vistula River to infect the rest of Poland.[50] Likewise, there has also been a consensus that the Black Death left the Kingdom of Bohemia unscathed, but there have been several challenges to that claim, most notably by the Czech historian Frantisek Graus. Graus has argued that although the Pestilence was not as severe in Bohemia during the 1348-1350 pandemic, it was still present. He also argued that by 1380, the Plague had hit Bohemia with full intensity.[51]
Little is known about the spread of the Plague through the Baltic States other than the fact that it did not appear in modern day Latvia until 1351. From there, it continued its eastward trek into Russia. Religious tension between the Muslim Golden Horde and Christian northern Russia resulted in a temporary reduction in trade between the two. Because the Plague followed established trade routes, the rest of Russia was temporarily spared until 1352, roughly five years after it initially appeared in the Crimea. Again, records are not very clear about the pattern of spread, but it is likely that the Plague entered Pskov from Latvia and then spread to Novgorod by 1352. There are no direct mentions of the Plague in Moscow, but the leader of the Russian Orthodox Church and the Grand Duke Simeon Gordiy of Muscovy and his seven children all died in 1353, leading historians to assume the cause of death was Plague.[52]
Overall, the Black Death killed between 30% and 50% of Europe’s population.[53] The mortality of the Plague was devastating to the population. The 14thcentury Carmelite friar Jean de Venette explained in his Chronicle that “Such an enormous number of people died in 1348 and 1349 that nothing like it has been seen or read about” and that “In many places, not two men remained alive out of twenty.”[54] The Pestilence continued to be epidemic in the following years, making its severity even worse. There were seventeen major epidemics in Europe until 1536. The Plague appears to have gone through a cycle that infected Europe roughly every eleven years.[55]
The Black Death Outside of Europe

Even though the Black Death’s impact on Europe is better known because of its considerable scholarly attention, it still had an equal impact on the Middle East.[56] According to the 14th century Muslim Historian Ibn Khaldun “In the middle of the eighth [fourteenth] century, civilization both in the East and the West was visited by a destructive plague which devastated nations and caused nations to vanish… Their [civilization’s] situation approached the point of annihilation and dissolution.” He even states that “The East, it seems, was similarly visited, though in accordance and proportion to (the East’s more affluent) civilization. It was as if the voice of existence in the world had called out for oblivion and restriction, and the world had responded to its call.”[57]
Both Latin and Arabic sources emphasize that the Plague originated in the Far East. From the Mongolian Steppes, the Plague spread outward, to both the south and the west. Just as throughout Europe, the Plague followed commercial trade routes. There were three main trade routes from the Far East to the Middle East. The first was an overland route from northern China and Mongolia through Turkestan to the Black Sea region. The second was a combined overland and sea route from China and India across the Indian Ocean and the Persian Gulf into Mesopotamia. The third was a sea route through the Indian Ocean up the Red Sea into Egypt. The Plague most likely followed the first route because there is no evidence of the Plague in Mesopotamia, Egypt, or India before it appeared in the Crimea.[58]
It is likely that the Black Death reached epidemic proportions in the Mongolian steppes around 1331. The widespread Plague would account for the death of Jayaatu Khan, emperor of the Yuan Dynasty, who died at the premature age of 28, along with his son.[59] However, there is little definite evidence of the Plague in China before the Qing Dynasty in the 17th century. The modern Chinese word for plague, shuyi, did not appear until the 19thcentury. Another issue with determining the effects of the Black Death in China was Chinese censuses counted houses, not people, so they are not an accurate representation of the population.[60]
Despite this, conjectures have been made that support the idea of the Black Death in China. The last two emperors of the Yuan dynasty, Jayaatu Khan and Ukhaantu Khan, were considered weak rulers. Their rules were characterized by rebellions, banditry, famine, and floods, which resulted in the withdrawal of the Mandate of Heaven, according to the Chinese. Epidemics were certainly part of the disasters associated with their rule. The first epidemic reported in China was in 1331, where it allegedly killed 90% of the province of Hebei’s population. There were three rounds of epidemics in the last forty years of the Yuan Dynasty. The best estimates predict that China’s population was 120 million in 1200, on the eve of the Mongolian invasion, and 60 million in 1390 when the Ming Dynasty replaced the Yuan Dynasty. Of course, some of the population loss was also due to the invasion itself, but the population likely grew after the Mongol invasions. Even considering death due to the other disasters associated with the late Yuan Dynasty, it is likely that mortality rate due to the Plague in China was comparable with the estimates made for Europe.[61]
The conquests of Genghis Khan in 1219 established an overland route to the Crimea from Otrar. By the 14thcentury, merchants heavily traveled the trade route. It is difficult to precisely trace the course of when and where the Plague spread from Mongolia to the Crimea, but an 1885 report by the Russian archeologist Daniel Abramovich Chwolson reported on two medieval Nestorian Christian cemeteries along Lake Issyk-Kul, in present day Kirghizstan, which contained headstones reporting 650 people who died between 1186 and 1349. 106 of the dead died in 1338 and 1339, and ten gravestones specifically mentioned pestilence as the cause of death.[62]
From approximately 1200 to 1760, central Asian Muslims controlled much of the northern plains of India and various parts of the rest of the subcontinent as well. The various dynasties often maintained significant commercial ties with Transoxiana and the Middle East, which both suffered greatly from the second plague pandemic. The Delhi Sultanate was the Muslim dynasty in control at the time of the Plague, and they had constant trade with central Asia and the Middle East. However, despite the close interactions, there is no record of a serious epidemic in India in the 14th century. Unlike the rest of the old world, India experienced significant population growth during the second half of the century. Therefore,the Plague likely did not enter India until the early 17thcentury, when it was making periodic reappearances in Europe and the Middle East.[63]
The Plague clearly struck the land of the Golden Horde in southern Russia between 1345 and 1346 where it was reported in Sarai and Astrakhan. From there, it spread to the Crimea and the Caucuses.[64] From Caffa in the Crimea, Italian merchants brought the Plague to Muslin Mediterranean. It probably reached Alexandria, Egypt’s principal port, in the late fall of 1347. It killed between 100 and 200 people a day within the first few weeks, but as the weather got colder, the mortality rate reached 750 deaths per day, and in the spring of 1348, it may have been as high as 1,000 a day. Alexandria’s pre-Plague population was around 100,000; it would not reach that point again until the 16th century. From the Nile delta, the pestilence spread throughout the Mamluk Sultanate. Cairo was struck by the Plague in the spring of 1348. Cairo was one of the largest cities in the world with a population of 500,000. Throughout the rest of 1348, at least 300 people died per day, and the death count reached as high as 7,000 a day. The city was in chaos; there was a shortage of coffins, shrouds, preachers, and gravediggers. Mass burials were performed in large open trenches. Mosques and shops were piled high with bodies. The Black Death continued to spread up the Nile to Aswan; it also spread eastward to Gaza, which served as a gateway to the rest of the Sultanate in Syria and Palestine.[65]
In late 1348, the Plague arrived in Antioch, a major commercial seaport. It is possible that the Plague traveled via trading vessels from Constantinople or Alexandria, or overland from Palestine. The mortality rate was at least 50% of the total population of 40,000. From Antioch and Palestine, the pestilence struck Damascus. Again, roughly half of the city’s 100,000 inhabitants died. Similar to many European accounts, the Syrian geographer Abu Hafs Umar ibn al-Wardi claims the mortality originated in China and India. He also similarly notes how the infected will cough up blood and will die after only two or three nights.[66] From Syria, the Black Death spread down the Arabian Peninsula and eventually reached the Muslims’ holiest city, Mecca. There are no reliable mortality rates, but the pestilence provoked theological debates because the prophet Muhammad claimed deadly diseases would never reach the Holy City. Many Islamic scholars blamed it on the presence of non-believers, which appears to have satisfied most of the Muslim faithful.[67]
The Plague spread to Persia and the Fertile Crescent from the Caucuses, further supporting the theory that the Plague did not enter the Middle East via India and the Indian Ocean. Sources date the arrival of the Plague in Azerbaijan to 1347. The pestilence spread to Baghdad from the north by the invading army of Malik Ashraf in 1347. The Plague interrupted the siege of the city, but it also infected it. The earliest mention of Plague in Armenia was in 1348 from monastery records in eastern Anatolia. The following year, there was widespread plague and famine in Armenia.[68]
The Black Death spread to North Africa from the Middle East by land and by ships from Egypt. It also likely spread via European merchants from Pisa, Genoa, and Sicily. Tunis, North Africa’s largest city was struck by the pestilence in spring 1348, where roughly 1,000 people perished daily. By 1349, all of the Middle East was inflicted by the Black Death. About a third of the entire population died.[69] Just as in Europe, the Plague continued to be epidemic during the next 200 years. It continually reoccurred roughly every nine years.[70]
The Medical Response in Europe

When the Black Death struck Europe in the middle of the 14th century, nobody knew how to prevent or treat the disease. Many believed they could cure it, but none of the bloodletting, concoctions, or prayers were successful. The overall intellectual framework of dealing with illness was flawed. The failure of medieval medicine is largely due to the strict adherence to ancient authorities and the reluctance to change the model of physiology and disease the ancients presented.[71]
14th-century medical theory and practice centered on the theories of the 4thcentury B. C. E. physician Hippocrates and the philosopher Aristotle as well as the 2nd century B. C. E. physician Galen. While these men moved human understanding of disease past mythological reasons, the physical explanations they gave were mostly incorrect. Christianity had little to say about the nature of the human body, so European physicians adopted Greek medical theories.[72] During the Middle Ages, there were no Greek versions of Galen’s texts available in Europe. Therefore, Europeans were forced to rely on Arabic translations.[73] Some of the translators became medical experts themselves. One of the most famous Muslim physicians is Ibn Sina (d. 1037). His The Canon of Medicine was used throughout Europe and the Middle East as a medical textbook. It was a summary of all medical and pharmaceutical knowledge up to his time.[74]
At the time of the Plague, Italy tended to be served by physicians the best. They were available in both cities and the countryside. Italian physicians were organized into a guild, and they treated everyone. France had about 1,700 physicians, but they mostly served only noble families. English physicians would often study in either France or Italy, but they were more similar to their French counterparts. In most European countries, there was a distinction between physicians, who had university training, and other practitioners, who were normally educated by an apprentice system.[75] Physicians had university training and were considered more proficient. Surgeons were educated by an apprentice system and carried out most surgical procedures. Barber-surgeons performed mainly minor surgeries.[76] All types of doctors utilized the services of pharmacists or apothecaries, who would prepare various herbs, minerals, pills, and concoctions for doctors. Apothecaries were respected and were powerful professionals, even though they were not university trained. Most people also had access to folk-healers, midwives, and other nonprofessional health care providers. In many cases, physicians were the least competent of all the health care providers, because of the education that gave them their high status. Their education was more theoretical and not practical.[77]
The first medical school in the Christian West is often ascribed to Salerno in southern Italy, but its origins are murky. A Benedictine hospital existed there from at least the 8th century. By the 10th and 11th centuries, Salerno was a hub of medical practice and scholarship.[78] As it developed throughout the 11th and 12th centuries, the hospital received the evolving Arabic medical doctrine from translations of Constantine the African and Jewish scholars in Toledo.[79] The Arabs placed a great emphasis on anatomy, which was beneficial to the medical profession.[80] Catholic education in general emphasized philosophy and was only mildly practical, so scholars relied on Greek and Arabic medical treatises.[81]
Unfortunately, any gains made by the emphasis on surgery and anatomy in Salerno were only temporary. The first public dissection in the Latin West took place in Bologna in 1281. The first dissecting manual, Anathomia, was published in 1316.[82] Church authorities limited or even flat out prevented the practice of autopsy. There were prohibitions against willfully destroying a human body. In 1300, Pope Boniface VIII passed a Bull forbidding the mutilation of bodies, even dead ones. Soon after, the medical faculty at the University of Paris declared that they were against surgery. Even at Montpellier, supposedly the most enlightened of the European medical schools, there was only one anatomy course every other year.[83] The only medical school to regularly teach dissections before the Black Death was the University of Padua.[84]
Most European Christians believed the origin of the Plague was from God, though some also said it was from Satan or the anti-Christ. They believed the Plague was sent for punishment of sins. Doctors accepted both spiritual and medical reasons for the Plague. They expected there to be multiple causes, and it was not a source of confusion. The belief that the Plague was God’s punishment was rooted in the Bible. Egypt received seven plagues in the Book of Exodus, in 2
Samuel 24, David punished his people with a Plague for carrying out a divinely forbidden census, and in 1 Samuel 5, those who stole the Ark of the Covenant were struck with painful swellings, similar to buboes. Some even believed the pain would have spiritual benefits; those who suffered on earth would be rewarded in the afterlife. The religious convictions did not stop physicians from treating the sick, for even though God sent the Plague, he also gave man tools to treat it. It was assumed that evil people for whom the Plague was sent for could not be cured. The belief that the Plague was an act of divinity continued up until the 17th century.[85]
The basis of medicine during the Black Death was the theory of humors.[86] Humoral theory is based on the idea that the Earth is composed of four elements: earth, water, fire, and air. Each element is linked to a bodily fluid, and each fluid assumes qualities of the elements. Fire is hot and dry and was associated with yellow bile. Air was associated with blood, so blood was assumed to be hot and moist. Phlegm’s element was water, which was moist and cold. Earth was
the element of black bile, which was thought to be cold and dry. Each humor was also associated with a color, a taste, an age, a temperament, and a season of the year.[87]

Astronomy, which was usually indistinguishable from astrology at the time, was commonly associated with medicine. Galen was an advocate for utilizing astrology with medicine. The Arabs also influenced European medicine with regards to astrology, even though by the time of the Plague, most Middle Eastern physicians did not believe in astrology.[88] Medical students often had access to astronomy experts. Astronomy/astrology was also an important part of the European medical education. At the University of Bologna, medical students were formally students of physica & astrologica and had a full curriculum of mathematics and astrology. This was also the case in many central and eastern European medical schools. At the University of Paris, medicine and astrology were not separated until 1537. In natural philosopher Albert the Great’s (d. 1280) “On the Causes and Properties of Elements,” he explains that air can be corrupted from celestial bodies. He says “For a conjunction of two stars in particular, which are Jupiter and Mars, with others assisting in the sign of Gemini, which is a sign of an airy triplicity, cause pestilent winds and corrupt air, which suddenly kill a large number of men and animals.” He backs up this argument by claiming that Jupiter is hot and moist, so it lifts up winds and vapors. Mars is hot and dry, so it ignites the vapors elevated by Jupiter. This causes lightening, pestilential vapors, and fires in the air, which leads to plagues.[89] These astrological theories were long-lived because they were considered scientific at the time, not mystical or religious. However, these explanations did have some contemporary critics. The German scholar Konrad von Megenberg (d. 1374) attacked astrological theories by stating a conjunction lasts only one or two years, but the Plague lasted for five.[90]
Along with astrology, Uroscopy and pulse-taking were the other common methods for diagnosis among physicians. Uroscopy was the principal diagnostic tool at the time. The color, texture, odor, and even taste of urine was analyzed. Often, a physician would take the patient’s sample of urine and compare it to other samples of urine either in flasks in the physician’s office or in medical textbooks.[91] Excess bodily humors were supposedly apparent in the urine.[92] Flasks were also compared with zodiac signs. Pulse-reading was featured heavily in Galen and Ibn Sina’s manuscripts, but was not generally as popular as uroscopy. Various rhythms of heartbeats could be classified as “bounding,” “formicant,” “vermicular,” or “gazelle-like.” The different rhythms were thought to be able to classify certain stages of diseases. Pulse-reading was often used in conjunction with uroscopy and astrology to develop a general diagnosis.[93]
Regardless of how God or the stars caused the Plague, most medical theorists believed the Plague was caused by bad air, or miasma. Both Hippocrates and Galen stated that bad air caused pestilence. The Arabs also accepted this theory, so it was the most orthodox model available to European physicians. Some blamed celestial bodies on the miasmatic air; others blamed it on earthquakes releasing poisonous gasses from the Earth. Earthquakes did precede some Plague outbreaks, so it is possible they disturbed rodent populations, causing them to come into closer contact to humans. Other earthly explanations for the miasma include southern winds, “exhalations” from swamps, decaying plants and animals, cesspools and sewers, dung heaps, and putrefied human corpses. The physician Gentile of Foligno (d. 1348) believed corrupt air could be released locally by opening long sealed caverns, wells, or even rooms in houses. This bad air was believed to be deadly.[94] Another proposed explanation stated in a medical treatise was that the poisonous air arose from the sea.[95]
Unlike their Muslim counterparts, most European physicians realized the Plague was infectious.[96] The friar Jean de Venette noted that “a healthy person who visited the sick hardly escaped death.”[97] John of Fordun’s (d. 1348) description of the Plague’s initial occurrence in Scotland describes how the Black Death “gathered such horror that children did not dare to visit their dying parents, or parents their children, but fled for fear of contagion as if from leprosy or serpent.”[98] Because of the belief in contagion, many physicians simply recommended leaving Plague-infested areas.[99]
Medical consilia were formal written communications in the form of explanations between physicians and patients who requested it. They were written for a nonmedical audience. Many of these medical tracts were produced during the Black Death.[100] One of the best known medieval Plague consilia is the 1365 treatise written by John of Burgundy.[101] In it, John of Burgundy begins by stating that everything made up of the elements is influenced by the heavenly bodies. He claims the heavenly bodies have corrupted the air. Many people have died from these evil vapors, especially those filled with evil humors. They die from both the outside air and the humors within them. John cites Galen by saying bodies will not be corrupted unless they have a tendency towards it. He claims cleansed bodies, free of evil humors, will not be afflicted by the Plague. He says the Plague will affect people differently depending on their astrological predispositions. He argues that many physicians are unable to treat the Plague because they are ignorant of astrology, “a science vital to the physician.”[102] Here John of Burgundy advocates both Galen’s humoral theory as well as astrology.
Because of the belief in miasmas, many preventative measures dealt with eliminating the poisonous air. It was believed that winds from the south generally were miasmatic, so houses were supposed to face north. The coasts were also shunned, which coincidentally did protect some, because the Plague was often imported via port cities. Marshes were also to be avoided because they were believed to have killing mists.[103] Some advocated keeping bad air out of one’s
home by sealing doors and windows tightly, though others said that keeping windows open would allow healthy air to enter houses. Holding one’s breath or breathing through a cloth when around the sick was also believed to help.[104] When the Plague was present, dry and richly scented woods were burned to keep the miasma at bay, including juniper, ash, vine, and rosemary. It was recommended that houses be filled with these pleasant smelling plants and aromas. If people had to leave their house when the Plague was present, a common precaution was to carry amber or a smelling apple,[105] which often contained amber, aloes, and rose water. Eau de Cologne, water from Cologne, and many perfumes had their origins in Plague stricken Europe. Gold was also thought to combat the sickness. It was believed gold contained power from the incorruptible sun and could purify any poison. Bathing in gold, or rose water for the poor, was thought to counteract the Plague poison.[106] In addition to gold, emeralds and pearls were also believed to have healing properties. Gentile of Foligno believed that powdered emerald was so potent that if a toad looked at it, its eyes would crack.[107]
One of the few precautions that actually was effective at preventing the Black Death was one mentioned by Dionysius Colle in the 16th century. He recommended throwing a powder consisting of sulfur, arsenic, and antimony into a fire. Sulfur is destructive to the bacteria, fleas, and rats.[108] Another example of preventative measures against miasmas is a 1371 butchery regulation in London. The regulations claim that the putrefied blood and entrails of slaughtered animals produced stenches that resulted in sicknesses among Londoners. The solution to combat the unnamed sickness was to require butchers to slaughter their animals outside the city.[109]
Humoral medicine dictated the avoidance of things that would moisten or heat the body. Hot baths would open pores, which could let corrupt material out, but they could also let it in, so they were to be avoided. Excessive exercise or sexual activity could heat the body and increase inhalation rates, causing people to breathe in more putrid air. Physicians also made a connection between mood and humoral balance. Negative feelings negatively affected the balance. It was recommended that emotions such as jealously, anger, sadness, and fear should be avoided. Likewise, positive emotions were believed to strengthen the heart against poisons.[110]
As for diet, physicians mostly suggested moderation and the avoidance of moist foods such as fish and milk. Heavily spiced “hot” foods were thought to be good.[111] The English poet John Lydgate (d. 1451) recommended abstaining from fruit. Poultry was beneficial, especially with sauces and spices. He also said not to eat raw foods, but to drink wholesome wine and eat white bread. Lydgate believed in the healing properties of rosewater, as well as sage and rue. He was also a strong proponent of moderation. He warned of overeating and eating late at night.[112] Many experts offered contradictory recommendations when dealing with food. The Granadan Muslim Ibn Khatimah (d. 1369) approved of fish, even though Lydgate advised against it. He also believed that eggplant and many fruits were safe, but few other medical experts agreed. Likewise, Gentile of Foligno was a proponent of lettuce, but the Faculty of Medicine at Paris forbade it.[113]
Bloodletting (phlebotomy, venesection) was very popular during the 14th and 15th centuries. Blood was the easiest humor to get to. Galen himself had allegedly been cured from a plague by bloodletting. Astrological considerations dictated the best time for a phlebotomy. Usually the best time was during the spring with a waning moon and a zodiac sign that was good for the patient.[114] An encyclopedia from a monastery in Cambridgeshire warned practitioners not to perform bloodletting on days divisible by five. Physicians and surgeons appeared to realize not to drain so much blood that it harmed patients. Normally, no harm resulted from bloodletting, and it may have actually been slightly beneficial as a preventative medicine because it encouraged periodic rest.[115] The buboes were thought to contain the Plague’s poison; therefore, various surgical techniques were utilized against them. Some advocated either piercing the buboes themselves, or drawing blood from around them. “Cupping” was another technique. A cup would be placed over a bubo and would then be heated, creating suction that was thought to suck the poison out. Likewise, numerous ointments were recommended because they were believed to draw the poison out.[116] The buboes were also often opened and cauterized.[117]
One of the most popular remedies for the Pestilence was theriac. Theriac was a complex mixture made up of many ingredients. It had been famous for being a universal antidote since ancient times, where it was used as a remedy for snakebites. It was very difficult to prepare; recipes would often contain up to eighty ingredients, and often, significant amounts of opium. Other ingredients included cinnamon, saffron, rhubarb, pepper, and ginger. The ingredients were mixed into a pulp, forming a thick, syrupy paste. Many physicians advocated the use of theriac. In 1348, the Paris Faculty recommended it to the king.[118] John of Burgundy prescribed consuming small amounts of it twice a week to prevent the Plague.[119] Contemporary reports also supported the effectiveness of theriac; Gabriel De’ Mussis noted that after a patient who was close to death was given theriac, the poison was expelled and the patient survived.[120]
The Black Death wreaked havoc on medical professions. Many physicians died working, either from the Plague itself or from exhaustion. Many followed their own advice and fled Plague areas. People criticized doctors for fleeing, being greedy, and for their inability to treat the Plague. Despite their critics, physicians and their consilia were in high demand throughout the couple of centuries following the Plague, revealing that they still maintained a high level of credibility, even though no major breakthroughs were made. Modern studies of the Black Death show that medieval doctors had little success. However, the physicians slowly moved away from their reliance on ancient authorities and toward their own observation and experience.[121]
The Medical Response in the Middle East

When studying the Black Plague in the Middle East, there is some confusion regarding terminology. There was one generic word for plague, which in addition to the Black Death, also could refer to cholera and other epidemic diseases. Not only is this a source of confusion today, but it was also confusing to Arab scholars of the medieval era. In a 1449 plague treatise by the Egyptian Ibn Hajar al-‘Asqalini, he complained that earlier writers did not properly distinguish between different diseases. They even included natural disasters such as drought, flood, and famine under the term “plague.”[122]
When the Plague struck the Middle East, the dominant view, inherited by Muslim scholars from earlier experiences of Plague epidemics, such as the Plague of Justinian, consisted of three principles: the plague was a mercy sent by God and a martyrdom for faithful Muslims, Muslims should not enter or flee areas stricken by the Plague, and there was no contagion because the disease came directly from God. All three traditions were attributed to the prophet Muhammad, who was reputed to have prohibited fleeing from a plague-stricken area. He also supposedly denied the pre-Islamic belief in contagion. Even though these precepts were common, they were not followed by everybody. There was a great flight from the countryside to the cities, resulting in rural depopulation during the Plague. There was also flight from the cities, most notably in Fustat. The Granadan physician Lisad-ad Din ibn Al-Khatib (d. 1374) was one of the few to support the contagion theory, but many of his peers disregarded him.[123]
Devout Muslims believed righteous and holy Plague victims were martyrs and would be taken directly to Paradise after their deaths.[124] Even though Muslims generally believed the ultimate cause of the Plague was the will of God, the manner that God caused the Plague to occur among men was the subject of many explanations. The majority of Muslim scholars were primarily interested in the theological explanation of the Plague; even the physicians who were more interested in physical causation were not free from the influence of religion in their explanations.[125] Non-Muslim physicians in the Middle East also had religious undertones. The Jewish physician Maimonides (d. 1204) said that having a healthy body is important because one has to be healthy to serve God.[126]
As in Europe, the dominant medical belief in the Middle East at the time was Galen’s humoral theory.[127] In addition to treating and preventing the Plague, Galen’s theory was used with regards to other medical problems. It was the foundation of much of the medical knowledge of the Middle East both before and during the Black Death. Galen’s theories were integrated into Arabic medicine once Baghdad was established in 762. Nestorian Christians, fluent in both Arabic and Greek settled in the new capital and translated Galen’s work into Arabic.[128] Galen was mentioned in a 9th century Nestorian dispensatory on the ideal hospital. The book mentions Galen’s quince wine that was supposed to help digestive problems.[129] It also advocates the use of Theriac, which it claims was originally used by Galen.[130] Another medical text, Abu al-Faraj ‘Ali ibn al-Husayn ibn Hindu’s (d. 1019) 11th century treatise, includes a history of the profession of medicine and states that the profession began in ancient Greece when a boy ate laurel seeds and then was bitten by a snake, but survived. The book then includes anecdotes by Galen of other examples of accidentally finding cures to poisons or diseases. their elemental counterparts.[131] He also discusses humors and[132] and mentions the lethality of pestilence, but offers no cure for it.[133] In a medical textbook by the Egyptian physician Abd al-Aziz al-Sulami (d. 1208), he references Galen’s work in determining pulses.[134] Al-Sulami also refers to one of Galen’s pills, al-quqaya, a mixture of aloe, scammony, colocynth pulp, and wormwood to expel humors from the body. book.[135] Galen is directly referenced in 34 of the 200 medical questions contained in the[136] When speaking of the best diet to promote health, Maimonides adopted Galen’s idea that vegetables were bad because they “do not possess good chymes.” He also was against the consumption of fruits unless one was sick.[137]
Just as in Europe, the most common theory of the Plague was the spread of corrupted air, or miasma. The miasma was believed to harm men, animals, water, and plants. The miasmatic theory was widely believed because it could be readily supported by religious beliefs and classical medical texts. Arabic writers adopted the theory either directly from Hippocrates and Galen or indirectly through other Muslim physicians, such as Ibn Sina. In Galen’s commentary of Hippocrates’s Epidemics I and III, he describes the idea of an energizing spirit, pneuma, which can be absorbed into the body through the atmosphere and is then radiated to the vital organs. This was a part of Galen’s humoral theory. The corrupt air was the result of a disturbance in the balance of the four elements, which then upsets the balance of the humors in an individual.[138] For example, in a medical treatise by Ibn Khatimah, he explains that the air humans breathe is not a pure element. It is a mixture of aqueous fumes, dry smoke developed from the earth, small particles of fire, and mostly elemental air. When air rots, the amount of elemental air is reduced relative to the other elements. This corrupted air can result in death if breathed in.[139] He gave three causes of Plague miasma: the irregularity of seasons, putrid fumes from decaying matter, and astrological events. He considered the first possibility to be the most likely. Ibn Sina stated that a sign of an approaching plague was when rats fled to the surface of the earth and died. However, he did not realize the causal relationship between the Plague and rats; he just believed rats perceived the miasma before men.[140] He also believed there were other environmental factors one could identify to warn of a forthcoming Plague. He thought climactic changes brought warm, moist southern air from the equator that carried Plague. Ibn Sina and other likeminded scholars believed they could predict the Plague by the colors of the evening sky, cloud formations, heavy rains, and violent winds.[141] Maimonides blamed the various plagues, pestilences, and famines that struck Fustat in the 11th century on putrid air.[142]
In Book IV of ibn Sina’s Canon, he describes how once the pestilent air reaches the heart, it rots the complexion of its spirit and then it rots the heart itself. An unnatural warmth then spreads through the body and a fever develops. Physicians believed the buboes were collection points for the poisonous material. Ibn al-Khatib believed buboes appeared mainly on the neck, armpit, and heart, because they corresponded with the brain, heart, and liver respectively. These were Galen’s three “emunctories,” the seats for the three human souls.[143]
One main difference between the Europeans and Arabs in regards to the cause of the Plague is that by the 14th century, the Arabs relied less on astrology.[144] There was some historical influence on astrology in medicine. Hippocrates and Galen admitted that astrology and medicine were relevant, but they never gave a scientific explanation as to how. The 9th century physician Abu Ma‘shar (d. 886) believed astrology had a great relevance in medicine. He said that each organ was associated with a specific planet and that celestial positions at the time of one’s birth determine their propensity to illness. medicine than even the Greeks did.[145] The Arabs initially incorporated more astrology into[146] Some of these ideas were certainly still present in the Middle East when the Black Death struck, but they were not prominent.[147] Ibn al-Khatib claimed the stars were outside the realm of medicine and Ibn Khatimah believed people did not know enough about the stars, so there was no point in relating them to medicine.[148] Even though many Muslim scholars rejected astrology, astrological explanations were more popular among the lower classes.[149] Physicians tended to focus more on the humors and environment when dealing with diseases because they could be modified easier than the celestial bodies.[150]
Even though many Muslim physicians refuted the theory of contagion on religious grounds, there still were a few physicians who believed in the contagion theory. Ibn al-Khatib recognized that outbreaks of Plague coincided with the arrival of contaminated men and that isolated communities, such as Muslim prisoners in Seville and North African nomads remained uncontaminated. The observable effect of pneumonic plague increased the belief of the interhuman transmission of the disease rather than miasma. The debate of miasma versus contagion lasted until the 19th century. The difference had a large effect on preventive medicine. During an outbreak of Plague in Egypt in 1834, the Europeans who believed the contagion theory, supported quarantine to reduce the spread of the disease, while the supporters of the miasmatic theory adhered to medieval Muslim plague treatises and believed the best way to prevent the spread was to change the air by fumigation. This was often done during the Middle Ages in both the Middle East and in Europe. Fires were lit at the mosque of at-Tannur in Cairo in times of Plague. Bonfires were set after the Great Plague of 1665 in London. There were also many compromises between the two theories of contagion and miasma, including the idea that infected people spread the sickness by way of a local miasma.[151]
While some authors of Plague treatises advocated for the benefit of medicine with regards to treating and preventing the Plague, there were many who believed the Plague was sent as a punishment from God and should simply be endured. Along with their medical instructions, most Muslim authors also recommended penance, supplication, and prayer. Throughout the Middle East, physicians relied on classical texts for information and treatment for the Plague, or derivatives of original treatises. One treatise cites the early Abbasid physician Yuhanna ibn Masawayh (d. 857), who claimed sucking an acrid pomegranate or plum and eating lentils, Indian peas, and pumpkin seeds in times of Plague. He suggested drinking sour fluids would keep the Plague away, as would eating a pickled onion every day before breakfast.[152]
Because Ibn al-Khatib believed in contagion, he recommended people stay away from the sick.[153] However, most other medical authorities believed in miasma, so many other preventative measures dealt with the problem of corrupted air.[154] Ibn Khatimah listed many ways to improve air quality and make people more resistant to the disease. First, he said one should seek fresh air, live in a house facing north, and surround oneself with cool fragrances such as myrtle and eastern aspen flowers. The house should be sprinkled with rosewater and lemon. People should rub themselves down with citron, lemon, roses, and violets. Drinking a mixture of aloes-wood with rosewater was also thought to prevent the disease. He also recommended avoiding the sun, warm winds, and ovens. He advocated keeping quiet and moderating movement would keep breathing rates down, which would prevent the spread of the Black Death. He also claimed that fruits, black and course bread, and meat cooked with lemon and vinegar were beneficial, while eggplant and garlic were to be avoided. Ibn Khatimah also warned against sleeping after meals and eating at irregular hours. It was believed that the scent from sweet smelling shrubs would prevent miasmatic air from reaching people. Open places were also believed to be deadly during epidemics. It was recommended that people stay indoors. Smoke and dirt were also thought to be able to overpower the Plague, which made people think that dirty areas were healthy.[155]
In order to cure those who became infected with the Plague, Ibn Khatimah advocated a number of concoctions, such as drinking a solution with Armenian clay. Armenian clay is a cure for the Plague directly mentioned by Galen that was also popular in Europe. Sometimes the clay itself was ingested, sometimes it was spread externally on the body. It furthermore was recommended that infected people should avoid constipation by eating cooked plums, violets, and tamarind. Lastly, Ibn Khatimah gave psychological advice to resist the Plague. He said it was important that the sick keep their morale up. This could be done by relaxing and avoiding sadness and excitement.[156]
Further treatments for the Plague included bloodletting in order to reduce fever and remove excess blood. Bloodletting was quite common in the Middle East as a cure for the Black Death. Ibn Khatimah was a supporter of bloodletting. He said it freed the life-force in the arteries. It was thought the Plague increased the amount of blood in its victims. Therefore, patients would often have five pounds of blood removed. Even after the initial Plague outbreak, bloodletting was still utilized. In 1449, Ibn Hajar advocated bloodletting as a cure.[157]
It also appears that the plague buboes were excised. Ahmed Tashköprüzade (d. 1561) mentioned that the Turks did not consider plague boils to be different from any other boil, and immediately removed them. Again, it was advised that bathing the buboes in a mixture of water and vinegar or rose, apple, mastic or myrtle oil would help. Cold water was also used to reduce pain. Some placed egg yolks on buboes. By the time the yolk dried, the bubo was expected to be healed. Many believed nothing was more beneficial than violets. Fruit juice was also often recommended, likely because dehydration was associated with the Plague.[158] The chronicler Ibn Taghribirdi (d. 1470) mentioned that sugar prices rose greatly when Plague broke out, as it was often prescribed as a medication. He also noted that few of the sick seemed to have been cured by sugar and other treatments such as purslane seeds and pears.[159]
Despite the apparent failure of Arabic medicine to effectively treat the Plague, it was still heavily influential on European medicine. European physicians were reliant on Arabic translations of Galen’s medical work. Christian crusaders were impressed by the Arabic hospitals. Pope Innocent III founded the hospital Santo Spirito in Rome in 1204. A network of hospitals then followed that appeared to have been modeled after Islamic hospitals in Cairo and Damascus.[160] Muslim medicine was also far more advanced in terms of surgery and dissection than European medicine. Church authorities prevented or limited the practice of autopsy. There were prohibitions against willfully destroying a human body, even a dead one. Many Muslims, on the other hand, agreed with the Andalusian polymath Ibn Rushd (d. 1198) that “whosoever becomes fully familiar with human anatomy and physiology, his faith in God will increase.” Despite the more advanced medical approach, Muslim physicians treated the Plague no better than Christian physicians.[161]
Islamic medicine was highly regarded in Christian Spain by both physicians and patients alike. Despite this fact, records indicate that only twelve physicians in the Kingdom of Aragon out of over a thousand were Muslim. This was a much lower percentage than the proportion of Muslims in the population as a whole. This fact may be because even though people respected Islamic medicine, they did not appear to respect Islamic doctors. It also may be the cause of Muslim practitioners leaving Christian lands. This was certainly the case of one Muslim physician, Muhammad al-Shafra. He was born in Crevillent, an independent Muslim enclave between Valencia and Murcia. When Crevillent was absorbed into the Kingdom of Valencia in 1318, he moved to Algeciras in the Muslim Kingdom of Granada. When that was conquered by Christians in 1344, he relocated across the straits of Gibraltar to Fez. Most other Islamic learned professionals in Christian Spain seemed to move south into Muslim lands where there were more opportunities for them.[162]
Jewish physicians were much more respected in Christian Spain. At the time of the Plague, the kingdoms in Spain were among the most tolerant towards Jews in Christian Europe. The expulsion of Jews from England and France in the late 13th and early 14th century resulted in an exodus of Jews immigrating to Aragon. Jewish physicians were highly regarded by both their patients and colleagues. Spanish Jews had a great reputation for medical learning and an intense intellectual reputation, which made Jewish medicine seem so attractive. There are many examples of Jewish physicians being highly regarded. Alazar Avinardut became a physician to King Alfons III in 1322. Alfons made no distinction between Christian and Jewish physicians. Avinardut also treated King Pere III’s sister, who said that he understood her health better than anyone else did. Both of Avinardut’s sons also served the kings of Aragon. Another example is in a letter to the queen from one of her servitors, A Jewish physician, Pere Folquet was named the best physician in Barcelona.[163]
Other Responses to the Plague

Even though many contemporary physicians wrote treatises on the cause of the Pestilence and how to treat it, there were many non-medical responses to the Plague in both Europe and the Middle East. In Europe, the most commonly held belief of the cause of the Plague was religious. European Christians viewed the Plague as a punishment from God for their sins.[164] This is evidenced in a letter of Robert Hathbrand, who was the Prior of Christchurch in Canterbury until 1370, to the Bishop of London. In the letter, Hathbrand explains that “[God] often allows plagues, miserable famines, conflicts, wars and other forms of suffering to arise, and uses them to terrify and torment men and so drives out their sins.”[165] Because the Plague came from God, many believed the best way to prevent the Plague was prayer. A letter of John Thoresby (d. 1373), Archbishop of York, states “it is important to urge, more devoutly and insistently, suffrages of devout prayer and other offices of pious propitiation, so that our Lord and God, pitying his people, may drive away all sickness.”[166] The Middle Eastern Muslims likewise believed the Plague was sent from God, but instead of believing it to be a punishment, some believed it to be a mercy from God and martyrdom for faithful Muslims.[167]
Based on biblical precedents, a conviction of personal guilt was engendered in many European Christians. This manifested itself as the flagellant movement in some. The movement was based on the belief that the mortification of flesh was considered a suitable penance for sins.[168] The “Brotherhood of the Flagellants,” as the movement was called, initially took root in Germany. The flagellants would march from town to town occasionally chanting hymns. Once they arrived in a new town, they would march around in a circle. When prompted by the master, they would throw themselves on the ground and would be whipped by him according to their sins. Then, they would stand and whip themselves with a heavy scourge with leather thongs and metal studs. The flagellants would continue to alternate between being on the ground, being whipped by a master, and standing, being whipped by themselves. While the flagellants brought a brief spiritual regeneration and the hope that the Plague would vanish when they initially arrived at a town, as a whole, they did more harm than good. New centers of infection rose in the towns, likely brought by the flagellants themselves. The newfound hope that they brought to the people they visited would also vanish soon after they left when the townsfolk realized that the sick were not cured and the Plague did not pass.[169]
Middle Eastern Muslims were more divided over the theological reason for the Plague. Many believed God sent the Plague to reward the faithful. Death by Plague was considered equal in God’s eyes to dying in battle; believers were assured of reaching paradise. However, likely influenced by Christians and Jews, some Islamic scholars considered the Pestilence to be a punishment from God. Accordingly, Muslim laws regarding alcohol and moral laxity were enforced more strictly during the epidemics of the 14th and 15th centuries. There was a whole spectrum of beliefs between the incompatible ideas that the Plague was sent by God as a reward and that it was sent by God as a punishment. Others believed the event to be neutral, decreed by an unknowable God. Regardless of the reason for the Plague, like European Christians, the Muslims had an increased emphasis on prayer, as well as personal piety and purity. There were many communal prayers for lifting the disease in larger cities. The lack of consensus about the divine reason for the Plague eliminated the possibility of a single ideological basis for social activism, such as the flagellant movement or the persecution of Jews in Europe.[170]
It was not just the Jews who were persecuted in Europe; lepers, Muslims, and foreigners were also accused of causing the Plague. However, the mass killings and persecution of the Jews during the Black Death were unprecedented in their extent and ferocity until the 20th century.[171] According to one account, between November 1348 and September 1349, all Jews between Cologne and Austria were killed for their crimes.[172] The attacks on Jews began after an accusation that they were responsible for the Plague by poisoning wells. A forced confession from ten Jews in Chillon in September 1348 was seemingly enough to implicate all European Jews. A second wave of persecutions arose in the middle of 1349, which was led by the flagellants and aided by masses of the poor.[173] They seemed to be oblivious to the fact that Jews died at least as frequently as Christians from the Plague.[174]
Despite the fact that a majority of the peasant Christians favored Jewish persecution and were convinced of the Jews’ guilt, the accusations were not taken seriously by most of the better-educated Christians. Other than a report from the Faculty of Medicine at Paris, who noted that the Plague may have been partially caused by polluted water from earthquakes, no contemporary scholars attributed the cause of the Plague to tainted drinking water. The rulers of Europe also attempted, though often unsatisfactorily, to protect their Jewish subjects.[175] Pope Clement VI argued that it was inconceivable that the Jews could have started the Plague. He forbade anybody to kill Jews or expel them from their homes on pain of excommunication.[176] Casmir of Poland appeared to have effectively halted Jewish persecution. Ruprecht von der Pfalz personally took many Jews under his protection, though only after receiving a handsome bribe. Other rulers who wished to assist the Jews were in no position to do so. After attempting to intervene, the patrician rulers of Strasbourg were overthrown by a mob. Pedro IV of Aragon had a high opinion of his Jewish subjects, but even after ordering that those who sacked a Jewish ghetto in Barcelona were to be punished, he was unable to stop the anti-Jewish rioting prevalent throughout his kingdom.[177]

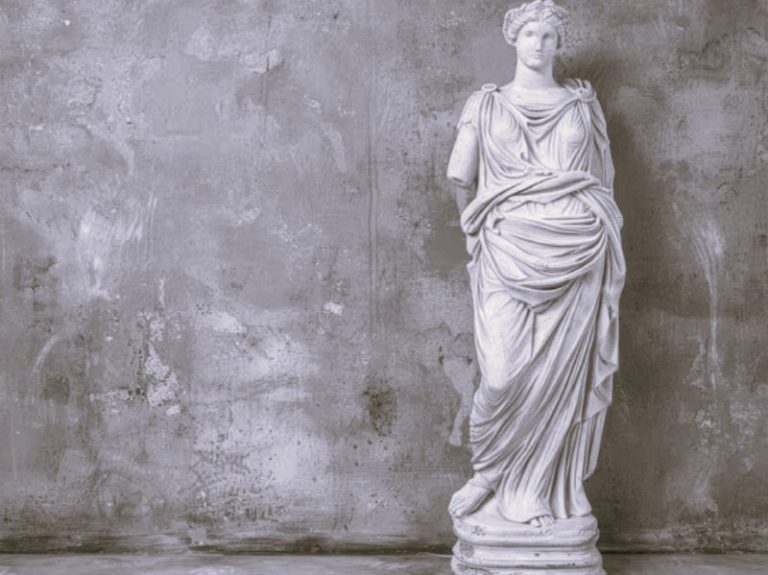
The Black Death also had a large effect on Medieval European culture. Death became more prevalent in art and literature. Tuscany was Europe’s financial center, and its ruling class became ingrained with a sense of independent inquiry in the arts. The art they favored was the “new” art of artists such as Giotto and Cimabue. This art tended to be uplifting, optimistic, and individualistic. When dealing with religious themes, preplague art emphasized the humility of Jesus, Mary, and the saints (Figure 2). The Tuscan bourgeois believed they could enjoy their temporal life without endangering their chance for salvation. All this changed after Tuscany lost around half of its population from the Black Death. New patrons after the Plague became more conservative, guilty, introspective, and moralizing. In Giovanni Del Biondo’s “St. John the Evangelist” (Figure 3), John is shown sternly trampling avarice, pride, and vanity, a very straightforward message. Art also became obsessed with the image of death.[178]

The dance of death was an allegorical theme that arose in the aftermath of the Black Death. As part of the allegory, the dead would rise up as skeletons and tempt the living to dance, resulting in their deaths. The allegory arose in the 14th century after the Plague. Paintings of the dance of death were painted on the walls of many churches, and it inspired the German painter Hans Holbein the Younger to make a set of 40 drawings featuring the dance (Figure 4).[179]

The Plague also resulted in the death of many scholars of the Latin language. This had opposite consequences in different areas. Because there was a scarcity of Latin teachers, vernacular languages began to be used in instruction. This helped bring forth a movement of cultural nationalism. However, beginning in Italy, there was also a movement to restore Latin to its classical purity.[180]
The Black Death also had a somber effect on literary styles of the time. This is evident in the works of Boccaccio. His literary masterpiece, The Decameron, was written in vernacular and was very popular. Its cynicism represented the common perception in the immediate aftermath of the Plague. The Decameron is largely guilt free, but his later works became much more somber. The Corbaccio, written in 1354-1355, is gloomier and more pessimistic as Boccaccio began to contemplate his own salvation. In his later years, Boccaccio actually condemned The Decameron. In northern European literature, the brevity of life was emphasized. There were also more references to the Old Testament, and it was stressed that God afflicted Plague upon both his chosen people and his enemies.[181]
The Black Death was a disastrous event on Europe and the Middle East. Even though it killed many, it still had a great effect on those who were not infected by the disease. This resulted in many religious responses to the Plague. There was more mass hysteria in Europe, which led the persecution of the Jews. Responses such as the flagellant movement reveal how the disaster affected the psyche of many individuals. This is also evident in the newfound pessimism in art and literature.
Effect on Medicine
Medicine slowly began changing during the generation after the initial outbreak of Plague. Many leading medical theoreticians perished in the Plague, which opened the discipline to new ideas. A second cause for change was while university-based medicine failed, people began turning to the more practical surgeons.[182] One example of this is the English surgeon John of Arderne (d. 1392), who served King Edward III. His Practica was based off years of experience, dealt with treatment and care, and was one of the most widely read post plague medical books. Together with several contemporary physicians, John of Arderne questioned medical dogma.[183]
With the rise of surgery, more attention was given to the direct study of the human body, both in sickness and in health. Anatomical investigations and dissections, seldom performed in preplague Europe, were pursued more urgently with more support from public authorities. French physician Guy de Chauliac (d. 1368) obtained the Pope’s permission to perform a[184] The dissection to identify the cause of the Plague before the Black Death subsided in Avignon. Chauliac ultimately failed to identify neither cause nor cure from his dissections, but it did serve to remove the stigma associated with surgery.[185] A slower, more far-reaching consequence of the Plague was that physicians slowly began to question the Galenic system of medicine.[186] Nothing concerning the Black Death could be found within Galen’s works, so doctors and laymen had to rely on their own wits and experiences to deal with the Plague.[187]
Another positive change associated with the publication of these newer medical works was that many were published in vernacular languages, instead of Latin, which allowed nonprofessional practitioners and the lay public to read them. Once the public had access to medical texts, the texts became demystified. The weakness of the preplague medical treatises became apparent to a wider audience, which further catalyzed the necessity of changes in the field of medicine.[188]
An additional positive impact after the initial outbreak was the new role of hospitals. Before the Plague, European hospitals were institutions solely designed to isolate the sick. They were more akin to today’s hotels rather than modern hospitals. The best care one could expect in a preplague hospital was warmth, cleanliness, and an adequate diet. After the Plague, a substantial number of hospitals began to try to cure their sick patients.[189] Hospitals also began developing associations with doctors. Before the Plague, only one hospital in Bury St. Edmunds was associated with a medical intern at Cambridge University. By 1450, all five of the town’s hospitals had a similar arrangement with local doctors.[190] Hospitals also became cleanlier. The best example of this comes from the Hotel Dieu in Paris. The walls of the hospital were washed biannually, bedding was washed and changed weekly, each ward had several bathtubs, and patients were cleaned weekly. Even though the hospital still would not be considered clean by modern standards, it was a large improvement over preplague hospitals.[191]
The Plague also led to developments in public health. Public health laws and the rise of municipal boards of health arose in Italy after the initial outbreak of Plague. From Italy, the concept of public health slowly spread throughout the rest of Europe. By the 16th century, public health was a common phenomenon in most of Europe’s large cities. The most effective board of health was in Milan. Milan had the lowest mortality rates of all other large Italian towns. Upon hearing of the Plague, the rulers of the city appointed a board of public health and gave it many powers. The board’s leaders were all noblemen, but the council was heavily staffed by medical professionals. The first job of Milan’s, and other boards, was to report the initial epidemic and then isolate it. After establishing a quarantine, which was not always successful, the boards would collect information from bills of mortality to help identify what the epidemic was and how to counteract it. By the late 15th century, these boards became so successful that many were granted similar powers to those of present day public health officials.[192]

In addition to, and often working with, the boards of health, a figure commonly associated with the Black Death, the Plague doctor (Figure 5) came to prominence. Beginning in Italy, and then spreading to France, England, the Netherlands, and Germany, town councils or public health boards would hire municipal physicians and surgeons specifically to treat Plague victims. It was a difficult and dangerous job. After treating victims, the Plague doctor would then be required to endure a long quarantine himself. Many doctors who volunteered for the job were either second-rate physicians who had trouble starting their own practices, or young physicians who were just starting out.[193]
The last major way European medicine began to develop after the Black Death was the evolution of medical ethics. Ethical codes, set by associations of medical practitioners dictated how medical professions were to act. In Arderne’s Treatises of Fistula in Ano, he advocated high standards of dress and appearance among doctors as well as professional courtesy. He recommended that surgeons have ready excuses not to take a case so they do not anger patients. In order for practitioners to be professional, they had to have prestige, a sense of power over the craft, and a good income.[194] Although Arderne often cared for the poor and needy and charged them less, he realized the importance of having a good income.[195] Again, in Treatises of Fistula in Ano, he said “the surgeon should always be aware of asking too little, for this is bad for both the market and the patient.”[196]
The Black Death did not have as large an impact on medicine in the Middle East as it did in Europe. One reason for this is that many of the improvements in European medicine had previously existed in the Middle East before the Plague, such as hospitals[197] and surgery.[198] Another reason the Plague did not have a large impact on medicine is because many Muslims were firm in their belief that the Plague was not caused by contagion. By the 16th century, when many European public health boards were issuing quarantines, Muslims regarded Christian health measures with disdain.[199]
Despite this, the Black Death still did have a positive influence on some aspects of medicine in parts of the Middle East. Medicine became more professionalized in the Ottoman Empire by the 16th century. These new physicians began to use empirical evidence with regard to the Plague. They made the distinction between the Black Death and other diseases that were also included under the term for plague. The Plague also resulted in a greater emphasis placed on hygiene in the Ottoman Empire. Because of miasmatic theory, dead animals and humans as well as garbage were considered sources of putrefaction that could cause disease. Foul smells in general came to be associated with miasma. This resulted in precautionary measures dealing with urban cleanliness.[200]
The Ottomans also began to challenge the notion that one should not flee Plague-stricken areas. This was not necessarily recommended because of a belief in contagion, but simply because they believed miasmas were sometimes localized within cities. Tashköprüzade stated that there was no harm in leaving a disease-infested area, so long as they did so in search of clean air or for preservation of health, and not specifically to flee the Plague. His opinions were approved by the judge Ebusuud Efendi (d. 1574). Ebusuud passed a legal opinion that authorized exiting cities infested with Plague to find a safe place. His opinion constituted Ottoman legal canon for centuries to come, legally allowing people to leave cities in times of Plague and other diseases.[201] Despite the fact that the Ottomans made improvements in public health and allowed people to flee areas stricken with disease, the only quarantines within the Ottoman Empire were run by European expatriates and the Greek minority within the Empire.[202] The Ottomans did not change their views on plagues and quarantines until persuaded by Europeans to do so in the 19th century.[203]
The rise of surgery, the positive transformation of the role of hospitals, the development of medical ethics, and the emergence of public health all helped advance the practice of European medicine. The Black Death also had a positive effect on Middle Eastern medicine, but the effect was not as pronounced. Modern medicine still had not developed during the initial or subsequent outbreaks of the Plague. Medicine required the triumph of physical sciences that came along with the scientific revolution to become truly modern. Even though this was not entirely accomplished until the 18th century, the foundations of modern European medicine were laid as a result of the Black Death.[204]
Conclusion
The Black Death, caused by the bacterial strand Y. pestis, wreaked havoc on much of the world in the 14th century. It likely began in the Mongolian steppes, but quickly spread throughout most of Asia and Europe, as well as parts of Africa. The Plague had mortality rates usually between 30% and 50%. Aside from the massive loss of life, the Plague was influential in many other ways.
The Black Death was influential on a multitude of disciplines. The epidemic greatly influenced religion in both Europe and the Middle East. Religion also played a large role in the response to the Plague. It also had an effect on European culture. Literature and pieces of art became much more somber and pessimistic in the years after the Plague. It would be advantageous for those who study Medieval art and literature to be knowledgable about the Plague. The effects of the Plague can also be studied with regards to psychology, sociology, and economics. One of the most obvious and important results of the Black Death is the effect that it had on medicine.
Middle Eastern and European medicine in the 14th century was based off theories of the Ancient Greeks Hippocrates, Aristotle, and Galen. The basis of Galen’s works was the theory of humors. It was believed that everything was made up of a combination of four basic elements and there was a body fluid that corresponded to each element. Because of the belief in humoral theory, moist and wet foods and objects were to be avoided. Many cures proposed by physicians dealt with balancing the body’s humors. A popular theory dealing specifically with the Plague was the theory of miasma, or corrupt air. The corrupt air was caused by a disturbance of the balance of the four elements. Preventative practices thus consisted of improving air quality and the avoidance of the miasmatic air.
Even though the basis of European and Arabic medicine were the same, there were still numerous differences between them. The Europeans still relied on astrology when dealing with medicine, while most Arabic physicians had abandoned the use of astrology. Muslims were also far more advanced in surgery and the study of anatomy than their Christian counterparts. There were regulations in the Christian West against the mutilation of bodies. Perhaps the largest difference between the two regions with respect to the Plague was that most Muslim physicians did not believe in contagion. The prophet Muhammad supposedly denied the pre-Islamic belief in contagion and thus prohibited fleeing from plague-stricken areas. The Europeans realized the contagious nature of the Plague and tried to establish quarantines.
As disastrous as the Plague was, it did at least have a positive effect on European and Middle Eastern medicine. In Europe, university based medicine failed to prevent or cure the Plague, so the populace began to place more trust in the practical surgeons. With the rise of surgery, more attention was given to the study of the human body. Physicians also slowly began to doubt Galenic medicine. To further promote the practice of medicine among those who were not university trained, many newer medical works were printed in vernacular languages. The Black Death also led to new roles of hospitals, the evolution of public health, and the development of medical ethics. This all served to advance the practice of medicine. Medicine was still not modern, it required the triumph of the physical sciences and the scientific revolution, but the foundations of European modern medicine were laid as a result of the Black Death.
The effects that the Plague had on Middle Eastern medicine is not as clear. There is a fair amount of research done on Plague within the Ottoman Empire, but outside the Ottoman Empire, research is really lacking. Just as in Europe, Ottoman physicians began to rely more on empirical evidence rather than texts from the ancients. Sanitation and hygeine were given a greater emphasis because of the miasmatic theory. The Ottomans also challenged the theory that people should not flee Plague-stricken areas. It would be very helpful to have more research done on the effects that the Plague had on medicine in the Middle East outside of the Ottoman Empire. More research on the Plague throughout the rest of Asia would also help to ascertain the results of the Plague. In both Europe and the Middle East, the most important effect was that doctors began to doubt Galen and relied more on empirical evidence. This alone was not enough to make medicine modern, but it certainly fostered medicine’s development.
Appendix
Endnotes
- The Middle East is a loosely defined region. In its current usage, the geographic term collectively refers to modern day Cyprus, Egypt, Iran, Iraq, Israel, Jordan, Kuwait, Lebanon, Saudi Arabia, Syria, Turkey, Yemen, Bahrain, Oman, Qatar, and the United Arab Emirates. When used to designate the area unified by Islamic law and custom, the term encompasses a larger area. In this paper, in addition to the lands included in the modern day geographic term, it also refers to North Africa and the Iberian Peninsula, as those areas were conquered by the Arabic Umayyad Dynasty by the 8th century. After the Umayyad Dynasty fell, the areas were still united through trade, scholarship, and the arts. Some medical scholars that were prevalent in Arabic medicine were from areas, such as Iberia, that today, are not considered to be part of the Middle East. Funk & Wagnalls New World Encyclopedia (2014), s.v. “Middle East,” accessed February 23, 2015, EBSCOhost.
- The best sources for research on the Black Death in Europe and the medical response are Robert S. Gottfried, The Black Death (New York: The Free Press, 1983), Philip Ziegler, The Black Death (London: Guild Publishing, 1991), and Joseph P. Byrne, The Black Death (Westprot, CT: Greenwood Press, 2004). For information regarding the spread of the Plague throughout Europe, see Ole J. Benedictow, The Black Death 1346-1353 (Rochester, NY: Boydell Press, 2004). Michael W. Dols, “The Second Plague Pandemic and Its Recurrences in the Middle East: 1347-1894,” Journal of the Economic and Social History of the Orient 22, No. 2 (May 1979) contains information both on the spread of the Black Death throughout the Middle East, as well as the medical response. Robert S. Gottfried, Doctors & Medicine in Medieval England 1340-1530 (Princeton: Princeton University Press, 1986) has information specific to England about doctors and the state of medicine both during and after the Black Death. Michael W. Dols, “The comparative Communal Responses to the Black Death in Muslim and Christian Societies,” Viator 5, (January 1974) discusses mainly non-medical responses to the Plague both in Europe and the Middle East.
- Gottfried, The Black Death, 6-7.
- Gottfried, The Black Death, 7.
- Gottfried, The Black Death, 7-9.
- Gottfried, The Black Death, 8.
- Norman Cantor, In the Wake of the Plague (New York: Harper Perennial, 2002), 12.
- Gottfried, The Black Death, 8.
- Gottfried, The Black Death, 8.
- Gottfried, The Black Death, 8.
- Ziegler, 18. While the description of the Black Death up to this point represents the ideas of most mainstream historians, it is still important to note that other theories of the Plague exist. There is an argument that some or even all deaths attributed to plague were actually caused by an anthrax outbreak. Cantor, 14. The historian Samuel Cohn Jr. argued in his The Black Death Transformed that written accounts of the Plague from the 14th century are inconsistent with 20th century accounts of the Plague. He therefore argues that the 14th century outbreak was not actually Plague. However, he does not propose an explanation of what the epidemic actually was, and his work has been criticized by other historians. M. R. McVaugh, review of The Black Death Transformed: Disease and Culture in Early Renaissance Europe by Samuel Cohn, Bulletin of the History of Medicine 78, no. 1 (Spring 2004): 212-214.
- Gottfried, The Black Death, 10-12.
- Gottfried, The Black Death, 15.
- Cantor, 8.
- Ziegler, 19.
- Gottfried, The Black Death, 15.
- William McNeill, Plagues and Peoples (Garden City, NY: Anchor Press/ Doubleday, 1976), 149-198, cited in Gottfried, The Black Death, 33.
- Gottfried, The Black Death, 33-34.
- Gottfried, The Black Death, 35-36.
- Gabriele de’ Mussis, Historia de Morbo, in Rosemary Horrox, The Black Death (New York: Manchester University Press, 1994), 16-17, accessed September 4, 2014, Manchester Medieval Sources Online. Despite this account, it is unlikely that catapulting dead bodies over the wall would have spread the Plague into Caffa, because of the mechanism of the spread of Y. pestis. It is more likely that insect and rodent hosts brought the Plague into the city. Gottfried, The Black Death, 37.
- Gottfried, The Black Death, 37.
- Byrne, 151.
- John VI Cantacuzenos, Historiarum, in Joseph P. Byrne, The Black Death (Westport, CT: Greenwood Press, 2004), 151-153.
- Benedictow, 74-76.
- Michele da Piazza, Cronaca, in Rosemary Horrox, The Black Death (New York: Manchester University Press, 1994), 35-36, accessed September 4, 2014, Manchester Medieval Sources Online.
- Gottfried, The Black Death, 42-44.
- De’ Mussis, 20.
- Gottfried, The Black Death, 44-46.
- Slavery had certainly existed in Europe before the year 1000 CE, but gradually disappeared during the 11th and 12th centuries with the increased population expansion. The labor shortage caused by the Plague caused Italian and Spanish merchants to import slaves from the Islamic east. Slavery also periodically existed in Europe after the Black Death, the Atlantic slave trade sent numerous slaves to the Iberian Peninsula, however, slavery was only utilized briefly in the 16th century and only in a few cities. Right after the Black Death was the only time after 1000CE when large numbers of slaves could be found throughout a large number of European cities. George Huppert, After the Black Death (Indianapolis: Indiana University Press, 1986) 112-113.
- Gottfried, The Black Death, 49-50.
- Gottfried, The Black Death, 51-53.
- Gottfried, The Black Death, 54-55.
- H. Geraud, ed., Chronique Latin de Guillaume de Nangis avec les continuations de 35 cette chronique, in Rosemary Horrox, The Black Death (New York: Manchester University Press, 1994), 55, accessed September 4, 2014, Manchester Medieval Sources Online.
- Gottfried, The Black Death, 56-57.
- J. F. D. Shrewsbury, A History of Bubonic Plague in the British Isles (Cambridge, UK: Cambridge University Press, 1970), 37-38.
- Gottfried, The Black Death, 58-64.
- Ziegler, 123-125.
- Henry Knighton and J. R. Lumby, ed., Chronicon Henrici Knighton, in Rosemary Horrox, The Black Death (New York: Manchester University Press, 1994), 77-78, accessed September 4, 2014, Manchester Medieval Sources Online.
- Shrewsbury, 39.
- Gottfried, The Black Death, 67.
- O’Donovan, trans., Annals of the Four Masters 3 (Cork, IE: CELT: The Corpus of Electronic Texts, 2002), 595596, accessed November 6, 2014, CELT: The Corpus of Electronic Texts.
- Gottfried, The Black Death, 67.
- Knighton and Lumby, 78.
- Shrewsbury, 45-46.
- Gottfried, The Black Death, 57-58.
- Benedictow, 216-218.
- Benedictow, 186.
- G. H. Pertz, ed. Monumenta Germaniae Historica –scriptorum IX, in Rosemary Horrox, The Black Death (New York: Manchester University Press, 1994), 61, accessed September 4, 2014, Manchester Medieval Sources Online.
- Gottfried, The Black Death, 68-69.
- Benedictow, 218-223.
- DC Mengel, “A Plague on Bohemia? Mapping the Black Death,” Past & Present 211, no. 1 (May 2011): 8-11.
- Benedictow, 209-214.
- Cantor, 7.
- Jean de Venette, Chronicle, in Rosemary Horrox, The Black Death (New York: Manchester University Press, 1994), 54-55, accessed September 4, 2014, Manchester Medieval Sources Online.
- Dols, “The Second Plague Pandemic and Its Recurrences in the Middle East: 1347-1894,” 169.
- Michael W. Dols, “The comparative Communal Responses to the Black Death in Muslim and Christian Societies,” Viator 5, (January 1974): 269-270.
- Ibn Khaldun, The Muqaddimah, Vol 1, trans. Franz Rosenthal (Princeton, NJ: Princeton University Press, 1980), 64.
- Michael W. Dols, The Black Death in the Middle East (Princeton: Princeton University Press, 1976), 38-44 accessed September 11, 2014, ACLS Humanities E-Book.
- Dols, The Black Death in the Middle East, 38-48.
- George D. Sussman, “Was the Black Death in India and China?,” Bulletin of the History of Medicine 85, no. 3 (Fall 2011): 344-345.
- Sussman, 345-349.
- Sussman, 327-328.
- Sussman, 332-335.
- Dols, The Black Death in the Middle East, 50.
- Gottfried, The Black Death, 38- 40.
- Abu Hafs Umar ibn al-Wardi, “Risalah al-Naba’ ‘an al-Waba,’” in Joseph P. Byrne, The Black Death (Westport, CT: Greenwood Press, 2004), 173-175.
- Gottfried, The Black Death, 40-41.
- Dols, The Black Death in the Middle East, 44-46.
- Gottfried, The Black Death, 41.
- Dols, “The Second Plague Pandemic and Its Recurrences in the Middle East: 1347-1894,” 168-169.
- Byrne, 33.
- Byrne, 34.
- Nigel J. Shanks and Dawshe Al-Kalai, “Arabian Medicine in the Middle Ages,” Journal of the Royal Society of Medicine 77, no. 1 (January 1984): 61.
- Funk & Wagnalls New World Encyclopedia (2014), s.v. “Avicenna,” accessed February 27, 2015, EBSCOhost.
- Byrne, 35-36.
- David Herlihy, The Black Death and the Transformation of the West (Cambridge, MA: Harvard University Press, 1997), 71.
- Byrne, 35-36.
- Jacalyn Duffin, “Salerno, saints, and Sutton’s Law: on the origin of Europe’s ‘First’ medical school,” Medical Hypotheses 73, No. 2 (August 2009): 265.
- Byrne, 34.
- Gottfried, Doctors & Medicine in Medieval England 1340-1530, 207-212.
- Byrne, 34.
- Byrne, 35.
- Ziegler, 51.
- Byrne, 35.
- Byrne, 38-40.
- Gottfried, The Black Death, 106.
- Dols, The Black Death in the Middle East, 86-87.
- Liana Saif, “The Arabic Theory of Astral Influences in Early Modern Medicine,” Renaissance Studies 25, no. 5 (November 2011): 610-612.
- Albertus Magnus, On the Causes of the Properties of the Elements, trans. Irven M. Resnick Milwaukee, WI: Marquette University Press, 2010), 110, accessed November 3, 2014, ProQuest Ebrary.
- Byrne, 42.
- Robert S. Gottfried, Doctors & Medicine in Medieval England 1340-1530, 170-178.
- Edward J. Kealey, Medieval Medicus (Baltimore: The Johns Hopkins University Press, 1981), 4.
- Robert S. Gottfried, Doctors & Medicine in Medieval England 1340-1530, 170-178.
- Byrne, 42-43.
- “A Fifteenth-Century Treatise on the Pestilence,” in Rosemary Horrox, The Black Death (New York: Manchester University Press, 1994), 193-194, accessed September 4, 2014, Manchester Medieval Sources Online.
- Byrne, 45.
- De Venette, 54-55.
- John of Fordun, Scotichorion, in Rosemary Horrox, The Black Death (New York: Manchester University Press, 1994), 84-85 accessed September 4, 2014, Manchester Medieval Sources Online.
- Ziegler, 52.
- Byrne, 36.
- Kari Anne Rand, “A Previously Unnoticed Fragment of John of Burgundy’s Plague Tract and Some Connected Pest Regimens,” Notes & Queries 53, no. 3 (September 2006): 295.
- John of Burgundy, The Treatise of John of Burgundy, in Rosemary Horrox, The Black Death (New York: Manchester University Press, 1994), 184-186, accessed September 4, 2014, Manchester Medieval Sources Online.
- Ziegler, 52-53.
- Byrne, 46-48.
- Ziegler, 52-53.
- Byrne, 46-48.
- Ziegler, 53-55.
- Ziegler, 52-53.
- H. T. Riley, Memorials of London and London Life in the XIIIth XIVth and XVth Centuries, in Rosemary Horrox, The Black Death (New York: Manchester University Press, 1994), 203-205, accessed September 4, 2014, Manchester Medieval Sources Online.
- Byrne, 48.
- Byrne, 48.
- John Lydgate, “A Diet and Doctrine for the Pestilence,” in Joseph P. Byrne, The Black Death (Westport, CT: Greenwood Press, 2004), 162-163.
- Ziegler, 53.
- Byrne, 49-51.
- Kealey, 4-6.
- Byrne, 49-51.
- Ziegler, 53.
- Christiane Nockels Fabbri, “Treating Medieval Plague: The Wonderful Virtues of Theriac,” Early Science and Medicine 12, No. 3 (January 2007): 248-263.
- Burgundy, 187.
- De’ Mussis, 25.
- Byrne, 51-52.
- Lawrence I. Conrad “Tāʿūn and Wabāʾ Conceptions of Plague and Pestilence in Early Islam,” Journal of the Economic and Social History of the Orient 25, No. 3 (1982): 271-272.
- Dols, “The Comparative Communal Responses to the Black Death in Muslim and Christian Societies,” 275-278.
- Byrne, 39.
- Dols, The Black Death in the Middle East, 84.
- Gerrit Bos, “Maimonides on the Preservation of Health,” Journal of the Royal Asiatic Society 4, No. 2 (July 1994): 215.
- Conrad, 275.
- Paulina B. Lewicka “Diet as Culture. On the Medical Context of Food Consuption in the Medieval Middle East,” History Compass 12, no. 7 (July 2014): 608.
- Sabur ibn Sahl, Dispensatory in the Recension of the Aḍudī Hospital, in Oliver Kahl, Islamic Philosophy, Theology and Science. Texts and Studies : Sābūr ibn Sahl’s Dispensatory in the Recension of the Aḍudī Hospital (Boston: Brill, 2008), 142-143, accessed October 23, 2014, ProQuest Ebrary.
- Sahl, 196-197.
- Abu al-Faraj ‘Ali ibn al-Husayn ibn Hindu, Key to Medicine and a Guide for Students, translated by Aida Tibi. (Reading, UK: Garnet Publishing, 2011), 31-32, accessed October 23, 2014, ProQuest Ebrary.
- Hindu, 60-61.
- Hindu, 76-77.
- Abd al-Aziz al-Sulami, Questions and Answers for Physicians, edited and translated by Gary Leiser and Noury Al-Khaledy (Boston: Brill, 2004), 33-39, accessed October 23, 2014, ProQuest Ebrary.
- Al-Sulami, 79-80.
- Al-Sulami, 10.
- Bos, 218-219.
- Dols, The Black Death in the Middle East, 85-87.
- Abi Gafar Ahmed ibn Ali ibn Khatimah, Tashil al-gharad al-qasid fi tafil al-marad alwafid, in Joseph P. Byrne, The Black Death (Westport, CT: Greenwood Press, 2004), 155-158.
- Dols, The Black Death in the Middle East, 88-89.
- Gottfried, The Black Death, 111.
- Bos, 225-226.
- Byrne, 43-44.
- Dols, The Black Death in the Middle East, 91-92.
- Saif, 610-614.
- Byrne, 34.
- Dols, The Black Death in the Middle East, 91-92.
- Byrne, 41.
- Dols, The Black Death in the Middle East, 91-92.
- Byrne, 34.
- Dols, The Black Death in the Middle East, 93-97.
- Dols, The Black Death in the Middle East, 98-99.
- Dols, The Black Death in the Middle East, 99-105.
- Conrad, 276.
- Dols, The Black Death in the Middle East, 99-105.
- Dols, The Black Death in the Middle East, 99-105.
- Dols, The Black Death in the Middle East, 105-106.
- Dols, The Black Death in the Middle East, 106-107.
- Lewicka, 611.
- Shanks and Al-Kalai, 61-64.
- Byrne, 35.
- Michael R. McVaugh, Medicine Before the Plague (New York: Cambridge University Press, 1993), 49-54.
- McVaugh, 51-63.
- Dols, “The Comparative Communal Responses to the Black Death in Muslim and Christian Societies,” 272.
- Robert Hathbrand, Terribilis, in Rosemary Horrox, The Black Death (New York: Manchester University Press, 1994), 113, accessed September 4, 2014, Manchester Medieval Sources Online.
- John Thoresby, Processions Against the Plague in 1361, in Rosemary Horrox, The Black Death (New York: Manchester University Press, 1994), 119, accessed September 4, 2014, Manchester Medieval Sources Online.
- Al-Wardi, 176.
- Dols, “The Comparative Communal Responses to the Black Death in Muslim and Christian Societies,” 273.
- Only a small minority of Europeans reacted to the Plague with such violence as the flagellants. However, they are worth noting because the fear and their desire to atone for their sins were present in many European Christians. Some may have thought the flagellants to be distasteful or dangerous, but no one thought their actions were meaningless or irrelevant. Ziegler, 64-71.
- Dols, “The Comparative Communal Responses to the Black Death in Muslim and Christian Societies,” 276-280.
- Dols, “The Comparative Communal Responses to the Black Death in Muslim and Christian Societies,” 274.
- Heinrich Truchess, The Persecution of the Jews, in Rosemary Horrox, The Black Death (New York: Manchester University Press, 1994), 210, accessed September 4, 2014, Manchester Medieval Sources Online.
- Dols, “The Comparative Communal Responses to the Black Death in Muslim and Christian Societies,” 274.
- Ziegler, 75.
- Ziegler, 71-78.
- Clement VI, Sicut Judeis, in Rosemary Horrox, The Black Death (New York: Manchester University Press, 1994), 221-222, accessed September 4, 2014, Manchester Medieval Sources Online.
- Ziegler, 78-80.
- Gottfried, The Black Death, 90-92.
- Funk & Wagnalls New World Encyclopedia (2014), s.v. “Dance of Death,” accessed March 10, 2015, EBSCOhost.
- Herlihy, 71.
- Gottfried, The Black Death, 92-93.
- Gottfried, The Black Death, 117-120.
- John Pearn, “Master John of Arderne (1307-1380): a Founder of Modern Surgery,” ANZ Journal of Surgery 82 no. 1/2 (January/February 2012): 48.
- Herlihy, 71-72.
- Geoffrey Marks, The Medieval Plague (Garden City, NY: Doubleday & Company, Inc., 1971), 137.
- Herlihy, 71-72.
- Erwin H. Ackerknecht, A Short History of Medicine (Baltimore, MD: The Johns Hopkins University Press, 1982), 90-91.
- Gottfried, The Black Death, 120.
- Faye Marie Getz, Medicine in the English Middle Ages (Princeton, NJ: Princeton University Press, 1998), 90, Accessed November 17, 2014, ProQuest Ebrary.
- Gottfried, The Black Death, 120-122.
- Gottfried, The Black Death, 120-122.
- Gottfried, The Black Death, 122-124.
- Gottfried, The Black Death, 125.
- Gottfried, The Black Death, 126-128.
- Pearn, 48.
- John of Arderne, Treatise of Fistula in Ano, in A. R. Myers, ed., English Historical Documents IV 1327-1485 (New York: Oxford University Press, 1969) 1184-1185.
- Shanks and Al-Kalai, 61-64.
- Byrne, 35.
- McNeill, 188-189.
- Nükhet Varlik, “From ‘Bête Noire’ to ‘le Mal de Constantinople’: Plagues, Medicine, and the Early Modern Ottoman State,” Journal of World History 24, no. 4 (December 2014): 765-767.
- Varlik, 767- 768.
- Birsen Bulmuş, Plague, Quarentines and Geopolitics in the Ottoman Empire, (Edinburgh, Scotland: Edinburgh University Press, 2012), 64.
- Bulmuş, 178.
- Gottfried, The Black Death, 128.
Annotated Bibliography – Primary Sources
- “A Fifteenth-Century Treatise on the Pestilence.” In Horrox, Rosemary. The Black Death, 193-194. New York: Manchester University Press, 1994. Accessed September 4, 2014. Manchester Medieval Sources Online. This treatise with an unknown author was featured in a 15th century compendium of medical texts. It contains an English translation of John of Burgundy’s treatise, one of the most widely read treatises on the Plague. The author confirms the belief that the Pestilence was a form of God’s vengeance. He also claims that the physical manifestation of the Plague originated from the sea. Lastly, the author states ways to protect oneself from the disease.
- Arderne, John of. Treatise of Fistula in Ano. In Myers, A. R., ed. English Historical Documents IV 1327-1485, 1184-1186. New York: Oxford University Press, 1969. John of Arderne was one of the most influential medieval English surgeons. He was a proponent of medical ethics and advocated that practitioners trust their own clinical experience. This excerpt includes him discussing the proper appearance of surgeons, the courtesies they should extend to their patients, and fees.
- Burgundy, John of. The Treatise of John of Burgundy. In Horrox, Rosemary. The Black Death, 184-194. New York: Manchester University Press, 1994. Accessed September 4, 2014. Manchester Medieval Sources Online. John of Burgundy’s Plague treatise was one of the earliest and widely read treatises on the Plague. In it, he advocates both humoral theory and astrology. He also discusses ways to prevent the disease and how to cure it. There is also a section regarding the practice of bloodletting.
- Cantacuzenos, John VI. Historiarum. In Byrne, Joseph P. The Black Death, 151-153. Westport, CT: Greenwood Press, 2004. John VI Cantacuzenos was the emperor of the Byzantines when the Black Death struck in 1347. He retired in 1355 and joined a monastery where he wrote a history of the Byzantine Empire from 1320 to 1347. Byrne’s The Black Death contains an excerpt from Cantacuzenos’ history. In it, he discusses symptoms of the Plague as well as the death of his son.
- Clement VI. Sicut Judeis. In Horrox, Rosemary. The Black Death, 221-222. New York: Manchester University Press, 1994. Accessed September 4, 2014. Manchester Medieval Sources Online. On July 5, 1348, Pope Clement VI reissued the papal bull Sicut Judeis. In the bull, Clement VI doubts that the Jews could be responsible for the Black Death. He also noted how many Jews themselves have died from the Pestilence. At the end, he forbids anybody to kill or expel Jews from their homes because of the Plague.
- Da Piazza, Michele. Cronaca. In Horrox, Rosemary. The Black Death, 35-41. New York: Manchester University Press, 1994. Accessed September 4, 2014. Manchester Medieval Sources Online. The Franciscan Michele da Piazza describes the arrival of the Genoese ships in Messina and the Plague they brought with them. A translated edition, originally from Rosarius Gregorio’s Bibliotheca Scriptorum qui res in Sicilia gestas sub Aragonum imperio retulere I, is included in Horrox’s The Black Death. This source is vital because it helps trace the progress of the Plague and shows how it likely arrived in Italy.
- De’ Mussis, Gabriele. Historia de Morbo. In Horrox, Rosemary. The Black Death. Gabriel de’ Mussis was a lawyer in Piacenza who witnessed the Black Death and recorded it in his Historia de Morto. Even though he was not actually on the ship that allegedly transported the Plague into Genoa, he still provides a contemporary account of both how the Plague arrived in Italy, and of the Plague itself. An excerpt of it is included in Horrox’s primary source compilation, The Black Death., 14-26. New York: Manchester University Press, 1994. Accessed September 4, 2014. Manchester Medieval Sources Online.
- Fordun, John of. Scotichorion. In Horrox, Rosemary. The Black Death, 84-85. New York: Manchester University Press, 1994. Accessed September 4, 2014. Manchester Medieval Sources Online. One of the few firsthand accounts of the Plague in Scotland. It is from John of Fordun, a clerk of Aberdeen. It appeared in W. F. Skene’s Chronica Gentis Scotorum in 1871, and again in Horrux’s The Black Death. It tells of how people died within two days of the first symptoms.
- Geraud, H., ed. Chronique Latin de Guillaume de Nangis avec les continuations de cette chronique. In Horrox, Rosemary. The Black Death, 54-57. New York: Manchester University Press, 1994. Accessed September 4, 2014. Manchester Medieval Sources Online. A part of the chronicle of the friar Jean de Venette that was written around 1560. The chronicle was published in French in 1843, and then was translated by Rosemary Horrux in The Black Death. The chronicle is written as though Jean de Venette wrote it, though he likely died in 1369. In it, it describes the effects of the Plague in Paris as well as the aftermath.
- Hathbrand, Robert. Terribilis. In Horrox, Rosemary. The Black Death, 113-114. New York: Manchester University Press, 1994. Accessed September 4, 2014. Manchester Medieval Sources Online. A letter from Robert Hathbrand, the Prior of Christchurch, Canterbury to the Bishop of London written in September 1348. The letter begins by saying God is in control of everything and that he makes men suffer to drive out their sins. Hathbrand continues by saying Edward III wishes everybody to pray for the protection of England.
- Hindu, Abu al-Faraj ibn. ‘Ali ibn al-Husayn. Key to Medicine and a Guide for Students. Translated by Aida Tibi. Reading, UK: Garnet Publishing, 2011. Accessed October 23, 2014. ProQuest Ebrary. An English translation of the original Arabic Muqaddimah, bu Ibn Khaldun. The monograph was originally written in 1377. It is a work of universal history, but also deals with Islamic theology, political theory, and natural sciences. The work consists of Ibn Khaldun’s description of the Black Death.
- Khatimah, Abi Gafar Ahmed ibn Ali ibn. Tashil al-gharad al-qasid fi tafil al-marad alwafid. In Byrne, Joseph P. The Black Death, 155-158. Westport, CT: Greenwood Press, 2004. A translated excerpt of Abi Gafar Ahmed ibn Ali ibn Khatimah’s 1348 medical treatise Tashil al-gharad al-qasid fi tafil al-marad alwafid was included in Joseph P. Byrne’s The Black Death. Khatimah was an Andalusian physician who described how an elemental imbalance can causes rotten air and water, which can lead to sickness. It is a very straightforward treatise that can be compared to European medical beliefs in that they are descended from Galen’s humoral theory.
- Knighton, Henry and J. R. Lumby. Chronicon Henrici Knighton. In Horrox, Rosemary. The Black Death, 75-80. New York: Manchester University Press, 1994. Accessed September 4, 2014. Manchester Medieval Sources Online. This firsthand account of the 14th century Augustinian canon Henry Knighton on the Black Detah in England appeared in Lumby’s Chronicon Henrici Knighton in 1895 and was included in Horrox’s The Black Death. The document tells of how the Plague first appeared in Bristol, but spread throughout England and Scotland. It also speaks of the reactions of the clergy and the economic effects of the Plague; how prices for many goods plummeted and how many buildings were vacant.
- Lydgate, John. “A Diet and Doctrine for the Pestilence.” In Byrne, Joseph P. The Black Death, 162-166. Westport, CT: Greenwood Press, 2004. A poem by the 15th century English poet John Lydgate. The poem lists several foods that were thought to be good at preventing the Plague, especially spiced poultry, bread made of good wheat flour, and wine in moderation. He also mentions multiple times that food in moderation is good. In addition to diet, he also advocates avoiding negative thoughts, public places such as baths and brothels, and excessive physical labor.
- Magnus, Albertus. On the Causes of the Properties of the Elements. Translated by Irven M. Resnick. Milwaukee, WI: Marquette University Press, 2010. Accessed November 3, 2014. ProQuest Ebrary. This Aristotelean commentary by Albert the Great was originally written sometime between 1251 and 1254. It was translated from its original Latin by Irven M. Resnick. The book is divided into two parts. The first part examines natural properties of the elements and the second half covers accidental properties. In the second part, Albert explains how astrological events can cause plagues. This primary document explains how medieval physicians relied on astrology.
- O’Donovan, John, trans. Annals of the Four Masters 3. Cork, IE: CELT: The Corpus of Electronic Texts, 2002. Accessed November 6, 2014. CELT: The Corpus of Electronic Texts. The Annals of the Four Masters is an anonymous text that spans the history of Ireland from the Great Flood to 1616CE. The annals are mostly a compilation of earlier annals. It covers major events in Irish history, and includes several entries that briefly discuss the Plague.
- Pertz, G. H., ed. Monumenta Germaniae Historica –scriptorum IX. In Horrox, Rosemary. The Black Death, 59-61. New York: Manchester University Press, 1994. Accessed September 4, 2014. Manchester Medieval Sources Online. An account of the Plague from the chronicle of the Austrian monastery of Neuberg that was published in 1851 and included in Horrox’s The Black Death. The chronicle blames the Plague on either the alignment of the planets or the corrupted air. It discusses the symptoms and effects of the Plague as well as the flagellants.
- Riley, H. T. Memorials of London and London Life in the XIIIth XIVth and XVth Centuries. In Horrox, Rosemary. The Black Death, 203-205. New York: Manchester University Press, 1994. Accessed September 4, 2014. Manchester Medieval Sources Online. Riley’s 1868 monograph contains a report of London butchery regulations in 1371. The regulations were included in Horrox’s The Black Death. The regulations come about because it was believed the air had been corrupted by the slaughtering of animals and the corrupted air was causing sicknesses.
- Sahl, Sabur ibn. Dispensatory in the Recension of the Aḍudī Hospital. In Kahl, Oliver. Islamic Philosophy, Theology and Science. Texts and Studies: Sābūr ibn Sahl’s Dispensatory in the Recension of the Aḍudī Hospital, 117-225. Boston: Brill, 2008. Accessed October 23, 2014. ProQuest Ebrary. Kahl’s monograph includes an introduction to Sabur ibn Sahl’s dispensatory on hospitals. It also includes the dispensatory itself in both English and Arabic. Ibn Sahl was a Nestorian physician in the 9th century who was one of the medical advisors to the Abbasid caliph al-Mutawakkil. In his text, he discusses the ideal hospital. He mentions many medicinal beverages and pills originally advocated by Galen. He also discusses Theriac.
- Sulami, Abd al-Aziz al-. Questions and Answers for Physicians. Edited and translated by Gary Leiser and Noury Al-Khaledy. Boston: Brill, 2004. Accessed October 23, 2014. ProQuest Ebrary. An English translation of Abd al-Aziz al-Sulami’s medical textbook. Al-Sulami was a physician and pharmacologist who was likely born in Damascus around 1155 and died in Cairo in 1208. His book contains answers to 200 medical questions. Thought there is no reference to the Black Death, al-Sulami is a proponent of Galen’s techniques, which reveals other humoral techniques the Arabs practiced.
- Thoresby, John. Processions Against the Plague in 1361. In Horrox, Rosemary. The Black Death, 119. New York: Manchester University Press, 1994. Accessed September 4, 2014. Manchester Medieval Sources Online. The preamble of a letter of John Thoresby, Archbishop of York’s, in 1361. Like most other Europeans, Thoresby believed the Plague was sent from God to punish humans for their sins. He thought the best way to eliminate the Pestilence was to pray to God for mercy.
- Truchess, Heinrich. The Persecution of the Jews. In Horrox, Rosemary. The Black Death, 208210. New York: Manchester University Press, 1994. Accessed September 4, 2014. Manchester Medieval Sources Online. An account of the persecution of the Jews by Heinrich Truchess, a canon of Constance. He begins by describing the confessions of Jews who allegedly poisoned well water to cause the Plague. He continues his account by describing the spread of the persecutions throughout Germany and Austria. Truchess wholeheartedly supports the murders of the Jews and calls for an end of all Jewish people.
- Venette, Jean de. Chronicle. In Horrox, Rosemary. The Black Death, 54-57. New York: Manchester University Press, 1994. Accessed September 4, 2014. Manchester Medieval Sources Online. A translated section of Jean de Venette’s Chronicle appeared in Rosemary Horrox’s The Black Death. Jean de Venette was a French Carmelite friar who wrote this section of the Chronicle around 1360. He describes the effect the Plague has had on France and the great mortality it caused. He also describes how some blamed the pestilence on infected air, and others blamed it on the Jews. This document is important because it is an example of the belief in the Plague spreading from person to person, as a contagion.
- Wardi, Abu Hafs Umar ibn al-. “Risalah al-Naba’ ‘an al-Waba.’” In Byrne, Joseph P. The Black Death, 173-177. Westport, CT: Greenwood Press, 2004. The Syrian geographer Abu Hafs Umar ibn al-Wardi gives a report of the Plague in Damascus. In his report, he describes how the Plague originated in China and India, and then traveled eastward and entered Europe through the Crimea before it infected the Middle East. He also mentions that a thousand people die every day. He discusses the symptoms of the Plague.
Annotated Bibliography – Secondary Sources
- Ackerknecht, Erwin, H. A Short History of Medicine. Baltimore, MD: The Johns Hopkins University Press, 1982. A revised edition of the monograph that was originally published in 1955. The book covers the history of medicine from Ancient Greece all the way to the 20th century. Because of its broad scope, it does not go into much detail on the Plague, but it does offer several paragraphs on the decline and rise of surgery in Europe as well as how the Plague affected the medical world.
- Benedictow, Ole J. The Black Death 1346-1353. Rochester, NY: Boydell Press, 2004. This monograph covers a comprehensive history of the Black Death from 1346 to 1353. It discusses the origin of the Black Death, its spread throughout the Middle East and Europe as well as mortality rates. Benedictow argues in it that contrary to previous sources, the Plague did not reach Iceland and it did infect both Poland and the Kingdom of Bohemia.
- Bos, Gerrit. “Maimonides on the Preservation of Health.” Journal of the Royal Asiatic Society 4, No. 2 (July 1994): 213-235.An article discussing the 12th century Jewish physician Maimonides. Just like his Islamic counterparts, Maimonides was strongly influenced by Hippocrates and Galen, and he had religious elements in his theories. The article includes a section on Maimonides’s belief in the miasmatic theory with regards to a Plague in Fustat.
- Bulmuş, Birsen. Plague, Quarentines and Geopolitics in the Ottoman Empire. Edinburgh, Scotland: Edinburgh University Press, 2012.A monograph discussing the Plague and quarantines within the Ottoman Empire. It discusses the medical response to the Black Death in the Ottoman Empire, and how quarantines were generally not utilized until the 19th century. The book focuses on the period after the initial epidemic in the 14th century, but it is still helpful with identifying the effect the Plague had on Turkish medicine.
- Byrne, Joseph P. The Black Death. Westport, CT: Greenwood Press, 2004. A monograph that covers the Plague, its effects on European society, and the psychosocial reactions to it. It also includes a modern medical perspective of the Plague as well as a medieval medical perspective. Towards the end of the book, it includes twelve primary documents, ranging from Italian wills to Arabic reports of the Pestilence.
- Cantor, Norman. In the Wake of the Plague. New York: Harper Perennial, 2002.Cantor’s book is divided into three sections. The first discusses the modern biomedical context of the Plague. The second is a social history of Europe right before and while it was suffering from the Black Death. The last covers both the aftermath of the Plague, as well as various other theories about it.
- Conrad, Lawrence I. “Tāʿūn and Wabāʾ Conceptions of Plague and Pestilence in Early Islam.” Journal of the Economic and Social History of the Orient 25, No. 3 (1982): 268-307. The primary focus of Conrad’s article is the specific definitions of Arabic words for plague. He discusses how there was not a specific term for the Black Death. His article also includes a section on the Arabic practice of Humoral Theory.
- Dols, Michael W. The Black Death in the Middle East. Princeton: Princeton University Press, 1976. Accessed September 11, 2014. ACLS Humanities E-Book.A monograph that discusses the Black Death as a whole in the Middle East. It includes the biomedical context of the Plague. It also discusses the spread of the Plague throughout the Middle East. There is a section devoted to the medical, religious, and magical interpretations of the Plague. Lastly, it discusses the consequences of the Black Death.
- —-“The comparative communal responses to the black death in Muslim and Christian societies.” Viator 5, (January 1974): 269-287.Dols discusses how much more scholarly attention has been giving to the study of the Black Death in Europe rather than in the Middle East. His article compares the communal response to the Plague in both Europe and the Middle East. The major differences between the two is that the Europeans believed in contagion, they thought the Plague was a punishment from God, and they advocated fleeing from Plague infested areas.
- —-“The Second Plague Pandemic and Its Recurrences in the Middle East: 1347-1894.” Journal of the Economic and Social History of the Orient 22, No. 2 (May 1979): 162189. An article discussing the recurrences of the Plague in the Middle East from 1347-1894. Dols discusses the various primary sources available that discuss the Plague. He also mentions the foci for the Plague that affected the Middle East and the Muslim response to the Plague.
- Duffin, Jacalyn. “Salerno, saints, and Sutton’s Law: on the origin of Europe’s ‘First’ medical school.” Medical Hypotheses 73, No. 2 (August 2009): 265-267. Duffin’s article is divided into three sections. The first and most useful section is about the alleged first European medical school at Salerno. The second section is about religious aspects of Salerno. The third section utilizes Sutton’s Law, “go where the money is,” to explain how priests and doctors gathered in Salerno.
- Fabbri, Christiane Nockels. “Treating Medieval Plague: The Wonderful Virtues of Theriac.” Early Science and Medicine 12, No. 3 (January 2007): 247-283.An article discussing theriac, one of the most popular remedies in medieval Plague medicine. The article discusses the composition and history of theriac. It also offers explanations as to why it continued to be used for so long.
- Getz, Faye Marie. Medicine in the English Middle Ages. Princeton, NJ: Princeton University Press, 1998. Accessed November 17, 2014. ProQuest Ebrary. A monograph that discusses the people and beliefs that made up English medicine between 750 and 1450. It discusses the variety of medical practitioners in England at the time. It also discusses medieval English medical texts. The book has several short sections on the Black Death, with one section regarding hospitals.
- Gottfried, Robert S. The Black Death. New York: The Free Press, 1983.This monograph describes the history of the Black Death before the 14th century as well as the environment of Europe and how it was favorable for the Plague to spread. It also discusses the spread of the Plague through Europe and the Middle East. Gottfried also mentions how the Plague changed European society and medicine. It is a great starting place for scholarly research on the Black Death.
- —- Doctors & Medicine in Medieval England 1340-1530. Princeton: Princeton University Press, 1986. Gottfried’s monograph discusses the history of English doctors and medicine from The Black Death to the foundation of the Royal College of Physicians. It discusses the prevalence of surgeons after the Plague and how it caused a shift in the practice of medicine.
- Herlihy, David. The Black Death and the Transformation of the West. Cambridge, MA: Harvard University Press, 1997. A monograph that discusses how the Black Death impacted and changed the Western World. He argues that the Plague led to new technological advances, helped establish new universities, and even led to the rise of nationalism. The book is important because it has a section clarifying the difference between surgeons and barber-surgeons. It also discusses the development of medicine after the initial epidemic of the Plague.
- Huppert, George. After the Black Death. Indianapolis: Indiana University Press, 1986. A monograph on the social history of Europe after the Black Death. It discusses ways that the Plague effected European society, including how it reduced the population of Europe and briefly reintroduced slavery to Europe.
- Kealey, Edward J. Kealey examines the medical practices in the first half of the 12th century. He describes the methods that doctors used to get diagnoses. He also discusses the rise and organization of larger hospitals. Even though this monograph discusses medicine before the time period covered by this paper, many of the medical practices, especially bloodletting, were used in the wake of the Plague, and they laid the foundation for medicine after the Plague.
- Lewicka, Paulina B. “Diet as Culture. On the Medical Context of Food Consuption in the Medieval Middle East.” History Compass 12, no. 7 (July 2014): 607-617.. Baltimore, MD: The Johns Hopkins University Press, 1981. An article that discusses the effects of humoral theory on the consumption of food as medicine in the medieval Middle East. It discusses some specific foods that were used to treat the Plague and other ailments, as well as the involvement of the Nestorians in translating Galen’s work into Arabic.
- Marks, Geoffrey. The Medieval Plague. Garden City, NY: Doubleday & Company, Inc., 1971. A monograph that covers the entirety of the second Black Death pandemic in Europe. It describes the spread of the Plague throughout the continent, as well as the responses of the doctors, priests, and people. There are also sections on the flagellants and the persecution of the Jews.
- McNeill, William. Plagues and Peoples. Garden City, NY: Anchor Press/ Doubleday, 1976. A monograph discussing epidemic diseases throughout history. The book is divided into six sections; from diseases of hunters and gatherers to improvements in medicine since 1700. The section from 1200-1500 is primarily concerned with the Black Death, both within and outside of Europe.
- McVaugh, Michael R. Medicine Before the Plague. New York: Cambridge University Press, 1993. A monograph discussing the medical practitioners and their patients in the Kingdom of Aragon from 1285 to 1345. The book also describes the success of the state of medicine in Spain. It also includes useful sections on Muslim and Jewish medical practitioners within the Christian Kingdom of Aragon.
- Mengel, DC. “A Plague on Bohemia? Mapping the Black Death.” Past & Present 211, no. 1 (May 2011): 3-34. An article that discusses and challenges the popular notion that the Black Death seemed to have skipped over the Kingdom of Bohemia. Mengel argues that the notion began in a map in a monograph by Elisabeth Carpentier in 1962. Since then, there has been little scholarly interest in the Plague in Bohemia. To support his thesis that the Plague was indeed present in the Kingdom of Moravia, Mengel largely referenced the Czech historian Frantisek Graus.
- Pearn, John. “Master John of Arderne (1307-1380): a Founder of Modern Surgery.” ANZ Journal of Surgery 82, no. 1/2 (January/February 2012): 46-51. An article on John of Arderne, a prominent post Plague English surgeon. The article includes a biography of him. It also discusses his Practica and his medical philosophy. John of Arderne is important in the development of English medicine because he challenged the work of Galen and advocated that surgeons trust their own clinical experience.
- Rand, Kari Anne. “A Previously Unnoticed Fragment of John of Burgundy’s Plague Tract and Some Connected Pest Regimens.” Notes & Queries 53, no. 3 (September 2006): 295-297. This article provides useful background information on the plague tract by John of Burgundy. The article says that this treatise is one of the best-known medieval treatises in English. Rand compares two versions of the Plague tract, both attributed to John of Burgundy.
- Saif, Liana. “The Arabic Theory of Astral Influences in Early Modern Medicine.” Renaissance Studies 25, no. 5 (November 2011): 609-626. An article discussing the historical astrological influences on Arabic medicine. It includes the Arabic theory of astrology and its relation to medicine. It also discusses the influences the Arabic astrological theories behind medicine had on European medicine.
- Shanks, Nigel J. and Dawshe Al-Kalai. “Arabian Medicine in the Middle Ages.” Journal of the Royal Society of Medicine 77, no. 1 (January 1984): 60-65. An article on the history and development of Arabic medicine. It describes the influence of Greek medicine and how they received Greek manuscripts from the Byzantines. The article also discusses the influence Arabic medicine had on European medicine. It describes how Europeans relied on Arabic translations of Galen’s texts and how many European hospitals were modelled after hospitals in Cairo and Damascus.
- Shrewsbury, J. F. D. A History of Bubonic Plague in the British Isles. Cambridge, UK: Cambridge University Press, 1970. A monograph on the Bubonic Plague in the British Isles. The book primarily focuses on the Plague in England, but also covers its effects in Scotland, Ireland, and Wales. It mainly deals with the initial epidemic of 1348, as well as the Plague in the 17th century. Shrewsbury also discusses the difficulties in identifying what epidemics were actual Plague epidemics and discusses other epidemic diseases that were also prevalent.
- Sussman, George D. “Was the Black Death in India and China?” Bulletin of the History of Medicine 85, no. 3 (Fall 2011): 319-355. Sussman discusses how many firsthand accounts of the Black Death in Europe and the Middle East assume the pandemic originated in Asia and infected China and India before arriving in the West. He discusses conjectures made that support the theory that the Plague began in China and Mongolia. He also refutes the idea that the Plague travelled through India before reaching the Middle East and Europe because there were no reports of the Plague in India until the 17th century.
- Varlik, Nükhet. “From ‘Bête Noire’ to ‘le Mal de Constantinople’: Plagues, Medicine, and the Early Modern Ottoman State.” Journal of World History 24, no. 4 (December 2014): 741-770. An article about the effect of Plague in the early Ottoman state. It discusses popular perceptions and scientific knowledge of Plagues before 1500, and then covers changing ideas of the Plague and how to prevent it. This article is very important in discussing the effect that the Black Death had on Middle Eastern medicine.
- Ziegler, Philip. The Black Death. London: Guild Publishing, 1991. A reprint of Ziegler’s original 1969 monograph. It contains information on the origin of the Plague and the state of Europe during the Plague’s outbreak. It also traces the path that the Plague took as it crossed Europe. It discusses the social, educational, and religious consequences of the Plague.
Published by James Madison University Libraries Scholarly Commons, Senior Honors Projects 2010-current, under the terms of a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International license.